The word cancer elicits many different feelings for people – fear, helplessness, and uncertainty just to name a few. Sadly, our fur babies aren’t immune from the grips of “the big C” but everyday we are learning more thanks to the efforts of researchers and board-certified veterinary oncologists. One of the most commonly diagnosed cancers in the dog world is lymphoma (7-24% of all dog cancers and 83% of all blood cancers in dogs). This week I have dedicated time to raising pet parent awareness about this cancer. It’s time to let a little air out of the balloon of fear that often elevates this cancer onto a pedestal on which it doesn’t deserve a place!
Lymphoma – What is it?
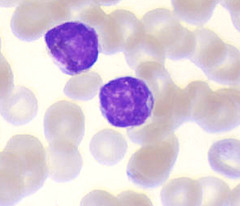
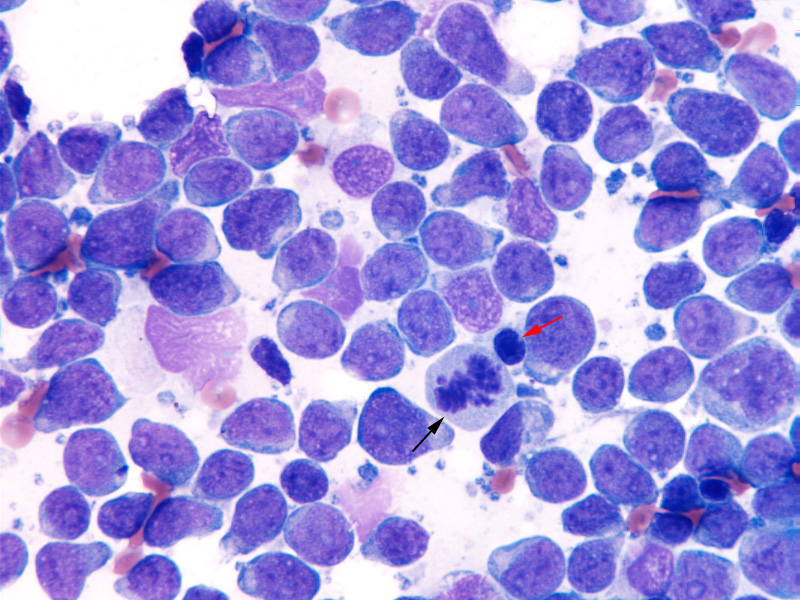
The term lymphoma (aka lymphosarcoma) is used to describe a type of cancer involving a specific white blood cell called a lymphocyte, as well as lymphoid tissue.
Lymphoid tissue can be found throughout the body, including in lymph nodes, spleen, liver, bone marrow, and digestive tract. Lymphocytes are a part of the immune system that protect the body from infection. There are two general types of lymphocytes – B cells and T cells – and both have been implicated in lymphoma.
Lymphoma can affect any body organ. Most commonly this cancer first becomes apparent in the main organs of the immune system, most notably lymph nodes, the spleen, and the bone marrow. There are five stages of lymphoma. The degree of peripheral (outside the body) and internal organ involvement defines a patient’s stage of lymphoma. Currently the World Health Organization (WHO) defines stages of lymphoma in dogs as follows:
- Stage I – involvement of only 1 peripheral lymph node on 1 side of the diaphragm (called focal lymphadenomegaly)
- Stage II – involvement of more than 1 peripheral lymph on the same side of the diaphragm (called regional lymphadenomegaly)
- Stage III – involvement of peripheral lymph nodes on both side of the diaphragm (called generalized lymphadenomegaly)
- Stage IV – involvement of liver and/or spleen
- Stage V – involvement of the nervous system, extranodal sites, and/or bone marrow
There are also five types of lymphoma:
- Multicentric (most common form) – lymphoma that most commonly affects the peripheral lymph nodes and may (or may not) involve other organs
- Mediastinal (rare) – lymphoma that originates from lymphoid tissue in the chest cavity
- Alimentary (~5% of patients) – lymphoma that originates from gastrointestinal tracts
- Cutaneous (uncommon) – lymphoma that originates from the skin
- Extranodal / Central Nervous System (rarest form) – the rarest form of lymphoma that involves organs like the eyes, bone, and mouth
Lymphoma – What causes it?
To date the definitive cause of lymphoma in dogs is not known. Discovering the cause (and ideally a cure) is a major focus of cancer research in both human and veterinary medicine. Some studies have identified risk factors for this cancer, including a weakened immune system, environmental factors, and exposure to certain chemicals (e.g.: paints, solvents, herbicides). Some breeds are seemingly over-represented, raising concerns for a genetic predisposition; these include:
- Golden Retrievers
- Boxers
- Basset Hounds
- Saint Bernards
- Airedales
- Bull Mastiffs
- Bull dogs
- Scottish Terriers
Lymphoma – What does it look like?
The clinical signs of lymphoma vary depending the type of lymphoma with which a patient is living.
- Multicentric – Patients living with this form of lymphoma commonly have painless enlargement of peripheral lymph nodes. Indeed, this lymph node involvement is often an incidental finding during a preventative healthcare examination. However, some dogs are sick with a variety of clinical signs including loss of appetite, weight loss, difficulty breathing, increased thirst, and increased frequency of urination.
Illustration of the location of peripheral lymph nodes in a dog. Image courtesy of www.marvistavet.com
- Mediastinal – This form of lymphoma commonly causes patients to have difficulty breathing. Affected patients may also develop swelling (edema) of the head, neck, and/or forelimbs.
- Alimentary – Patients with this form of lymphoma commonly have clinical signs referable to the gastrointestinal tract, particularly vomiting, diarrhea, weight loss, loss of appetite, increased thirst, and increased frequency of urination.
- Cutaneous – Lymphoma of the skin typically starts as dry, red, flaky, and itchy patches of skin. However, as the disease progresses, patients develop reddened ulcers, nodules, and/or plaques lesions on the skin.
- Extranodal / Central Nervous System – The clinical signs for this form of lymphoma depend on the site of disease. Patients with lymphoma in the central nervous system may be profoundly weak or paralyzed; they may also have seizures. Patients with lymphoma in the eyes can have visual impairments. Those with bone lymphoma may limp, have difficulty finding a comfortable position, and self-restrict their physical activity.
Lymphoma – How is it diagnosed?
There are several methods for obtaining a definitive diagnosis of lymphoma, ranging from non- and minimally invasive techniques to more invasive surgeries. Most commonly a veterinarian will perform either a fine needle aspiration or a surgical biopsy. What’s the difference?
Fine Needle Aspiration (FNA) with Cytology: An FNA is inexpensive and easy to perform. There is low risk to the patient, and sedation is typically not needed. A veterinarian uses a needle that is the size used to give a vaccination, so there is essentially no discomfort for the pet. Lymph nodes, as well as internal organs, can readily be aspirated under most circumstances. Samples are then evaluated by a board-certified veterinary clinical pathologist – this evaluation is called cytology. Unfortunately, cytology is not a perfect – it is not always accurate! Board-certified veterinary oncologists and internal medicine specialists perform FNA procedures routinely. Partnering with one of them can be quite helpful for maximizing obtaining a diagnostic sample.
Surgical Biopsy: Given the potential limitation of aspiration with cytology, occasionally a surgical biopsy of affected tissue is required to obtain a definitive diagnosis. A biopsy is a minor surgical procedure to remove a piece of lymph node or other organ affected by cancer. In general, the larger the biopsy sample, the better the chance for an accurate diagnosis of lymphoma. Many family veterinarians are comfortable performing the necessary biopsy procedures. With that being said, partnering with a board-certified veterinary surgeon can be invaluable for ensuring the most appropriate tissue sample is obtained.
After making a definitive diagnosis, some additional testing is recommended to determine how involved the body is with the cancer. These tests also tell veterinarians if a pet has other medical conditions that could affect treatment decisions and overall prognosis. This testing process is called staging, and recommended tests include:
- Complete blood count – a non-invasive blood test that provides information about red blood cells, white blood cells, and clotting cells called platelets
- Biochemical profile – a non-invasive blood test that provides information about liver and kidney health, as well as electrolytes (e.g.: sodium, potassium) and gastrointestinal enzymes
- Urinalysis – a non-invasive urine test to help assess kidney function and to screen for infection in the urinary tract
- Chest radiographs (x-rays)
- Abdominal imaging (radiographs/x-rays +/- sonography)
- Bone marrow sampling – a minimally invasive procedure to look for evidence of lymphoma in bone marrow
- Fine needle aspiration with cytology for organs that appear abnormal via sonography
- Immunophenotyping – minimally invasive test to determine the type of lymphocyte causing a patient’s lymphoma
Lymphoma – How is it treated?
Lymphoma, in general, is most effectively treated with chemotherapy. I understand that word elicits intensely negative feelings in most of you. I get it. Yet please try to understand chemotherapy for pets is remarkably different (read better) from anti-cancer treatments for humans. I previously dedicated some time discussing this important difference – please read more by clicking here. In addition to chemotherapy, some patients benefit from other forms of therapy, including surgery and/or radiation therapy.
Pet parents should also understand lymphoma is rarely cured. Most commonly this cancer goes into remission. What does this mean? Remission is simply defined as causing a regression of cancer, and can be partial (cancer burden has been reduced by at least 50%) or complete (cancer is undetectable). There are numerous chemotherapy protocols for lymphoma, and many factors are considered when selecting the most appropriate anti-cancer treatment plan for a pet. Many factors influence remission rates and survival times, including:
- Primary cancer site
- How sick a patient is at the start of chemotherapy
- Blood calcium level
- Presence of lymphoma in the bone marrow
- B cell versus T cell lymphocytes (aka immunophenotype)
Currently, anti-cancer protocols associated with the highest rates of remission (70-95%) and longest overall median survival times (9-14 months) involve combinations of drugs given over several weeks to months. Median survival time means 50% of patients will live beyond this time point and 50% will die before reaching it. Dogs with multicentric lymphoma treated with the most aggressive anti-cancer drug protocol have an average survival time of one year, and approximately 20% live longer than two years. Consultation with a board-certified veterinary oncologist or internal medicine specialist is instrumental in selecting the best chemotherapeutic plan for your fur baby.
Unfortunately, most dogs will experience a relapse of their cancer at some point. Achieving a second remission is possible, but it is usually of shorter duration than the first remission because the cancerous cells become resistant to the effects of chemotherapy. Eventually most lymphomas develop resistance to all chemotherapy drugs, and dogs with lymphoma die or are euthanized due to an unacceptable quality of life.
The take-away message about lymphoma in dogs…
Lymphoma, a cancer of a type of white blood cell called a lymphocyte, is one of the most common cancers that afflicts dogs. Any organ of the body may be affected, and clinical signs vary depending on the site(s) involved. This cancer is most effectively treated with chemotherapy, and many patients will achieve remission with treatment. Partnering with a board-certified veterinary oncologist or internal medicine specialist is uniquely beneficial to ensure your pet is diagnosed and treated accurately, efficiently, and effectively.
Wishing you wet-nosed kisses,
cgb
To find a board-certified veterinary oncologist or internal medicine specialist, please visit the American College of Veterinary Internal Medicine.