Those who consistently read my blog know I love blood. That’s sounds weird, doesn’t it? Yet, it’s true. Blood is awesome – platelets, clotting factors, white blood cells, and of course, red blood cells! This week I’m dedicating space to share info about erythrocytosis or too many circulating red blood cells. It’s an intriguing abnormality, and I hope you find the material helpful. Happy reading!
Erythrocytosis – What is it?
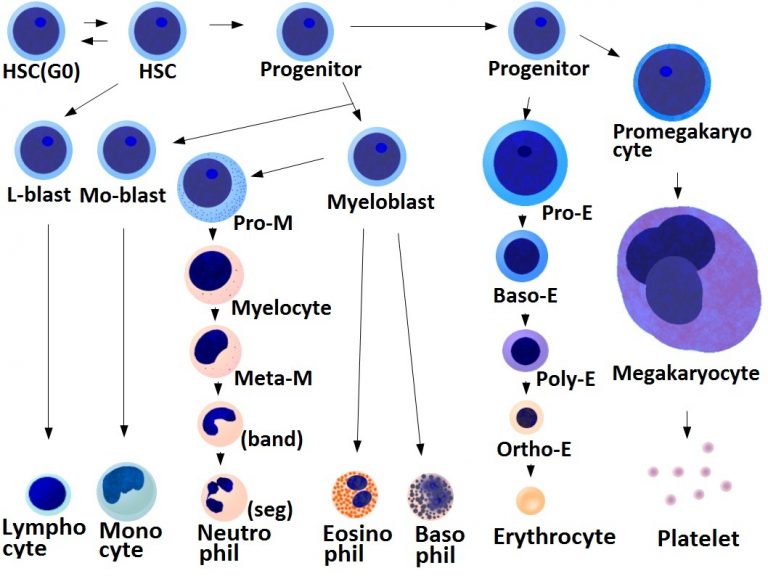
To understand erythrocytosis, one must have a basic understanding of the formation of red blood cells. This process is called erythropoiesis. Red blood cells transport oxygen throughout the body. When the body senses low oxygen, the kidneys produce a hormone called erythropoietin. Major reasons for low systemic blood oxygen are:
- Anemia
- Heart and lung diseases
- Altered blood flow to the kidneys
- Reduced atmospheric oxygen (e.g.: living at high elevations)
Erythropoietin stimulates the medulla of bone marrow to make red blood cells and secrete them into circulation. Erythropoiesis also occurs in the liver and spleen under certain circumstances. This is called extramedullary erythropoiesis. When too many red blood cells are released into circulation, the resulting condition is called erythrocytosis. The terms erythrocytosis and polycythemia are often used interchangeably and will be used as such throughout this post.
Erythrocytosis – Why does it occur?
Blood is composed of red blood cells and plasma. When the volume of plasma decreases relative to the concentration of red blood cells, the percentage of red blood cells increases even though the actual number hasn’t increased. There is no increase in erythropoiesis. Erythropoietin levels are unchanged. This condition is called relative erythrocytosis. Common causes include dehydration and water loss due to reduced intake, vomiting, diarrhea, and increased urination.
Erythrocytosis caused by enhanced erythropoiesis is called absolute erythrocytosis. This condition is characterized by either increased or normal erythropoietin production. The former is called absolute secondary erythrocytosis while the latter is called absolute primary erythrocytosis or polycythemia vera.
Absolute secondary polycythemia is subcategorized as either appropriate or inappropriate. Conditions that should cause increased levels of erythropoietin are termed appropriate, and include:
- Congenital heart disease (e.g.: ventricular septal defects, tetralogy of Fallot, reverse patent ductus arteriosus)
- Upper airway obstruction
- Chronic lung disease
- Brachycephalic airway syndrome
- High altitudes
Inappropriate absolute secondary conditions are characterized by elevated erythropoietin levels in the absence of low systemic oxygen. These conditions include:
- Erythropoietin-producing kidney tumors
- Hyperthyroidism
- Hyperadrenocorticism (Cushing’s disease)
- Liver cancer
- Polycystic kidney disease
- Necrotizing pyelonephritis
- Kidney cysts
- Pheochromocytoma
- Cecal leiomyosarcoma
Absolute primary polycythemia – also called polycythemia vera – is a rare bone marrow disorder caused the abnormal proliferation of red blood cells in the bone marrow independent of erythropoietin concentration. In people and in some dogs, there is a mutation in a gene called JAK2. This mutation causes an increased sensitivity of the erythropoietin receptor in the bone marrow.
Erythrocytosis – How is it diagnosed?
Documenting an elevated percentage of red blood cells is straightforward, requiring only a simple blood test called a packed cell volume (PCV). However, properly characterizing the type of erythrocytosis requires a:
- Thorough patient history
- Complete physical examination
- Diagnostic testing

A complete physical examination is an important step in the diagnosis of erythrocytosis (U.S. Air Force photo/Airman Alexis C. Frost)
Veterinarians may recommend a series of logical tests include:
- Blood assays (e.g.: complete blood count, biochemical profile)
- Urinalysis
- Diagnostic imaging (e.g.: chest & heart sonography, abdominal sonography)
- Blood gas testing
- Erythropoietin testing – unfortunately, this test is not currently available in the United States
- Bone marrow sampling
Pet parents will likely find it invaluable to consult with a board-certified veterinary internal medicine specialist to develop a logical and cost-effective diagnostic plan for their fur baby.
Erythrocytosis – How is treated?
Definitive treatment for erythrocytosis ultimately depends on the type. For example, patients with relative erythrocytosis benefit from the replacement of the fluids they’ve lost. Those with absolute polycythemia often require periodic removal of blood. This is called therapeutic phlebotomy. Pets with polycythemia vera typically receive a medication call hydroxyurea to reduce excessive red blood cell production by the bone marrow. Pet parents are encouraged to partner with a board-certified veterinary internal medicine specialist to determine the best treatment for their pet.
The take-away message about erythrocytosis in dogs and cats…
Erythrocytosis or polycythemia is defined as an increase in circulating red blood cells. There are many potential causes, and a proper diagnostic investigation. With timely identification and appropriate treatment, many patients can lead high quality lives.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
CriticalCareDVM