Like humans, our pets can experience allergic reactions. Most of them are mild in nature, but some may be life-threatening. My hope is this week’s post will raise awareness about allergic reactions so pet owners are better able to respond to these potentially serious life events. I hope you find the information helpful – happy reading!

What are allergic reactions?
To understand allergic reactions, one needs to have a basic understanding of immunology. Any substance to which the body is exposed that causes the body’s immune system to react is called an antigen. Antigens are typically proteins, for example those found in venom of various insects. Antigens – sometimes called allergens – enter the body through the skin, respiratory tract, gastrointestinal tract, and/or by injection. Common antigens include:
- Venoms from insects (i.e.: bee stings)
- Drugs (i.e.: antibiotics, chemotherapeutic agents, etc.)
- Vaccines
- Blood product transfusions
When first exposed to an antigen, the body’s immune system produces a special antibody called immunoglobulin E (IgE). The IgE then binds to a type of white blood cell called basophils in the bloodstream and to a similar type of cell called mast cells in the tissues. This initial exposure is usually not associated with any clinical signs, but does make the pet more sensitive to the allergen in the future – this process is called sensitization. Occasionally, a pet can have an allergic reaction during initial exposure if a large amount of antigen is present.
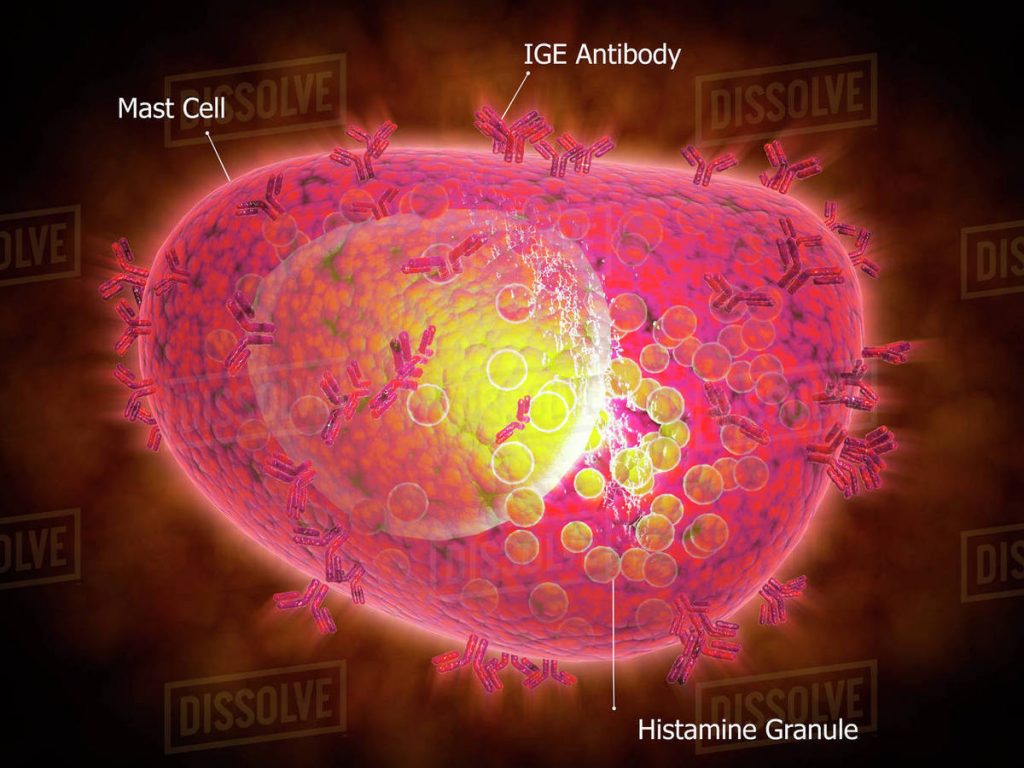
More commonly, hhen sensitized animals subsequently encounter the antigen, basophils and mast cells with IgE on their surface release substances like histamine, prostaglandins, and leukotrienes that cause swelling or inflammation in the surrounding tissues. These reactions range from mild to severe.
What do the look like?
As you may imagine, there are different types of allergic reactions. In fact, there are four types:
- Type I – Anaphylaxis
- Type II – Antibody interaction with normal tissue antigens
- Type III – Arthus reaction
- Type IV – Delayed hypersensitivity reaction
A type I or anaphylactic reaction is what most pet owners think of when they imagine an allergic reaction. Thankfully, it’s rare in dogs and cats. Pets develop urticaria (also known as hives), focal itchy skin swellings. Dogs and cats also develop angioneurotic edema, which is non-itchy swelling of tissue beneath skin of the pinnae (ear flaps), lips, nose/muzzle, and eyelids. In dogs, anaphylaxis targets the liver while in cats the respiratory tract and gastrointestinal tracts are predominantly affected. As such, vomiting, diarrhea, respiratory distress, collapse, and death can occur. An important point to remember is anaphylaxis can happen the first time a pet encounters a large amount of an allergen.

Drugs and vaccines can trigger any of the four types of hypersensitivity reactions. Drug allergies often manifest three or more days after exposure. Clinical signs include:
- Skin lesions – rashes, ulcerations, scabs/crusts
- Fever
- Joint swelling / immune-mediated polyarthropathy
- Protein-losing nephropathy (PLN)
- Immune-mediated hemolytic anemia (IMHA)
- Immune-mediated thrombocytopenia (ITP)
How are allergic reactions diagnosed?
The diagnosis of an allergic reaction is typically made based on both compatible history and clinical signs. For example, the development of facial swelling and hives immediately after administering a vaccine is consistent with a type I hypersensitivity reaction.

To definitively confirm a specific substance (i.e.: drug, vaccine, etc.) is the cause of a pet’s allergic reaction, one technically needs to satisfy specific criteria, specifically:
- The antigen causes clinical signs in a patient
- Clinical signs resolve with removal of the antigen
- Clinical signs recur with reintroduction of the antigen
Realistically, the third criterion is rarely satisfied due to the concern for a severe reaction with reintroduction of an allergen.
How are they treated?
Anaphylaxis and severe drug reactions requires immediate emergency treatment in a veterinary hospital. These patients may require supplemental oxygen, intravenous fluid therapy, temporary breathing support, and various injectable medications. Patients with mild clinical signs can often be treated on an outpatient basis with an antihistamine and tapering dose of a corticosteroid. Whenever possible, the confirmed or suspected antigen should be removed and avoided in the future.
The take-away message about allergic reactions in dogs and cats…
Allergic reactions can be triggered by a wide variety of substances collectively called antigens. Some reactions of very mild and self-limiting while some are life-threatening and ultimately fatal without timely appropriate intervention.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
Wishing you wet-nosed kisses,
CriticalCareDVM