Atrial fibrillation and atrial flutter are common supraventricular tachyarrhythmias in dogs. Both conditions impair atrial function and can reduce cardiac output. Early identification and decisive treatment can improve patient comfort and clinical outcomes.
Pathophysiology
Atrial fibrillation develops when the atria generate rapid, disorganized electrical impulses that bombard the atrioventricular (AV) node that conducts them irregularly to the ventricles. Ventricular response rates often rise above 160 beats per minute (bpm) in dogs with structural heart disease. High sympathetic tone in heart failure patients further increases the ventricular rate. The loss of coordinated atrial contraction reduces preload and can worsen cardiac output.
Two clinical forms are well recognized.
Lone atrial fibrillation occurs in large and giant breed dogs with structurally normal hearts. Their large atria support reentrant circuits that allow the arrhythmia to persist. Ventricular response rates are often normal or only mildly elevated because the AV node filters many fibrillatory impulses.
Secondary atrial fibrillation occurs in dogs with structural cardiac disease, such as dilated cardiomyopathy (DCM) or advanced AV valve degeneration. These patients often have atrial dilation and high sympathetic tone, which contribute to rapid ventricular response and worsening heart failure.
Atrial flutter generates organized macro reentry circuits within the atria. Atrial rates often exceed 300 bpm. Many impulses are blocked at the AV node, producing 2:1 or 3:1 conduction patterns. Untreated atrial flutter can progress to atrial fibrillation.
Clinical Signs
Many dogs with lone atrial fibrillation appear bright at rest. Some dogs show reduced stamina during exercise. Dogs with structural heart disease often present with coughing, tachypnea, weakness, or collapse.
Diagnosis
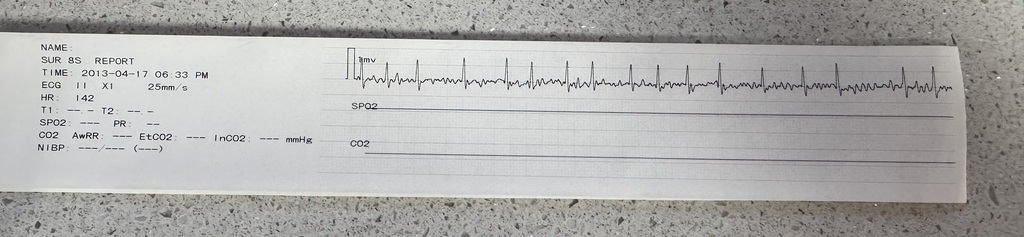
A thorough cardiovascular examination and high quality ECG are essential.
Key findings on ECG include:
• Atrial fibrillation: irregularly irregular rhythm without identifiable P waves. Fibrillatory waves may be present.
• Atrial flutter: sawtooth flutter waves best seen in leads II, III, and aVF. Ventricular response depends on AV nodal conduction.
• Rapid ventricular rate in structural heart disease patients.
• Normal or mildly elevated rate in lone atrial fibrillation.
Echocardiography determines whether the arrhythmia is associated with structural disease. Thoracic radiographs help identify cardiomegaly or pulmonary edema. A Holter monitor is valuable for follow up after treatment.
Treatment Goals
Lowering the ventricular response rate improves diastolic filling and cardiac output. Restoring sinus rhythm can improve atrial function in appropriate candidates. Treatment decisions depend on the presence of structural heart disease, ventricular response rate, arrhythmia duration, and the patient’s stability.
Pharmacologic Management
Rate control therapy
Rate control is the standard approach for dogs with structural heart disease. These patients have a short-lived return to sinus rhythm after cardioversion and face higher anesthetic risk.
• Diltiazem (0.5-1.5 mg/kg PO q8 hr) can slow AV nodal conduction. Extended release forms are effective when administered at 3-4 mg/kg PO q12 hr.
• Digoxin can be combined with diltiazem for improved rate control. The dose for dogs is 0.003-0.005 mg/kg PO q12 hr. Careful monitoring of serum digoxin concentration is essential.
• Dogs in congestive heart failure also receive diuretics, ACE inhibitors, and pimobendan.
Pharmacologic rhythm control
Most drugs used for rhythm conversion are unreliable for canine atrial fibrillation. Dogs with lone atrial fibrillation may receive diltiazem before cardioversion to lower the ventricular response and improve safety.
Synchronized Electrical Cardioversion
Synchronized cardioversion is the most effective strategy for restoring sinus rhythm in dogs with lone atrial fibrillation. It is rarely recommended for dogs with structural heart disease due to limited long term success and increased risks. Cardioversion requires a biphasic defibrillator with a synchronized mode. The system analyzes the R wave and delivers energy precisely at ventricular depolarization. This precise timing prevents shock delivery during the T wave, which could induce ventricular fibrillation.
Step-by-step instructions
- Pre-procedure preparation
Clip and clean the right and left lateral thorax over the atria. Place two large defibrillator pads or paddles with conductive gel.
Confirm the diagnosis with a high quality ECG.
Perform baseline blood pressure and cardiac assessment.
Fast the dog and plan general anesthesia. The shock is uncomfortable and requires complete patient immobility. - Anesthesia
Induce anesthesia with an agent compatible with cardiovascular stability. Maintain with inhalant anesthesia. Provide oxygen and continuous ECG monitoring. - Positioning and equipment setup
Place the patient in right lateral recumbency.
Attach the ECG leads from the defibrillator to ensure optimal visualization of the R wave.
Select synchronized mode on the defibrillator. Confirm the device displays clear synchronization markers on each R wave. - Energy selection
Begin with 1-2 joules/kg using a biphasic waveform. Lower energy requirements are typical with biphasic shocks. - Delivering the shock
Apply firm pressure on the paddles if using hand-held paddles.
Warn the team to stand clear.
Deliver the synchronized shock.
Observe the ECG for immediate rhythm conversion. - Re-synchronization between shocks
Some devices revert to unsynchronized defibrillation mode after shock delivery.
Always confirm that synchronized mode is still active before delivering any additional shock. - Additional shocks
If sinus rhythm is not restored, increase energy in small increments.
Reassess pad placement and contact. - Recovery
Once sinus rhythm is restored, discontinue anesthesia and monitor the patient until fully recovered.
Repeat ECG before discharge.
Schedule follow up ECG or Holter monitoring to assess rhythm stability.
Treatment of Atrial Flutter
Atrial flutter may respond to antiarrhythmic therapy, but many cases require synchronized cardioversion. Dogs that convert successfully often transition into stable sinus rhythm. The decision to proceed with cardioversion follows the same principles used for atrial fibrillation.
Prognosis
Dogs with lone atrial fibrillation often enjoy excellent quality of life after successful cardioversion. Recurrence is possible, especially in dogs with atrial enlargement. Dogs with structural heart disease rely on rate control therapy to improve comfort and slow progression of heart failure.