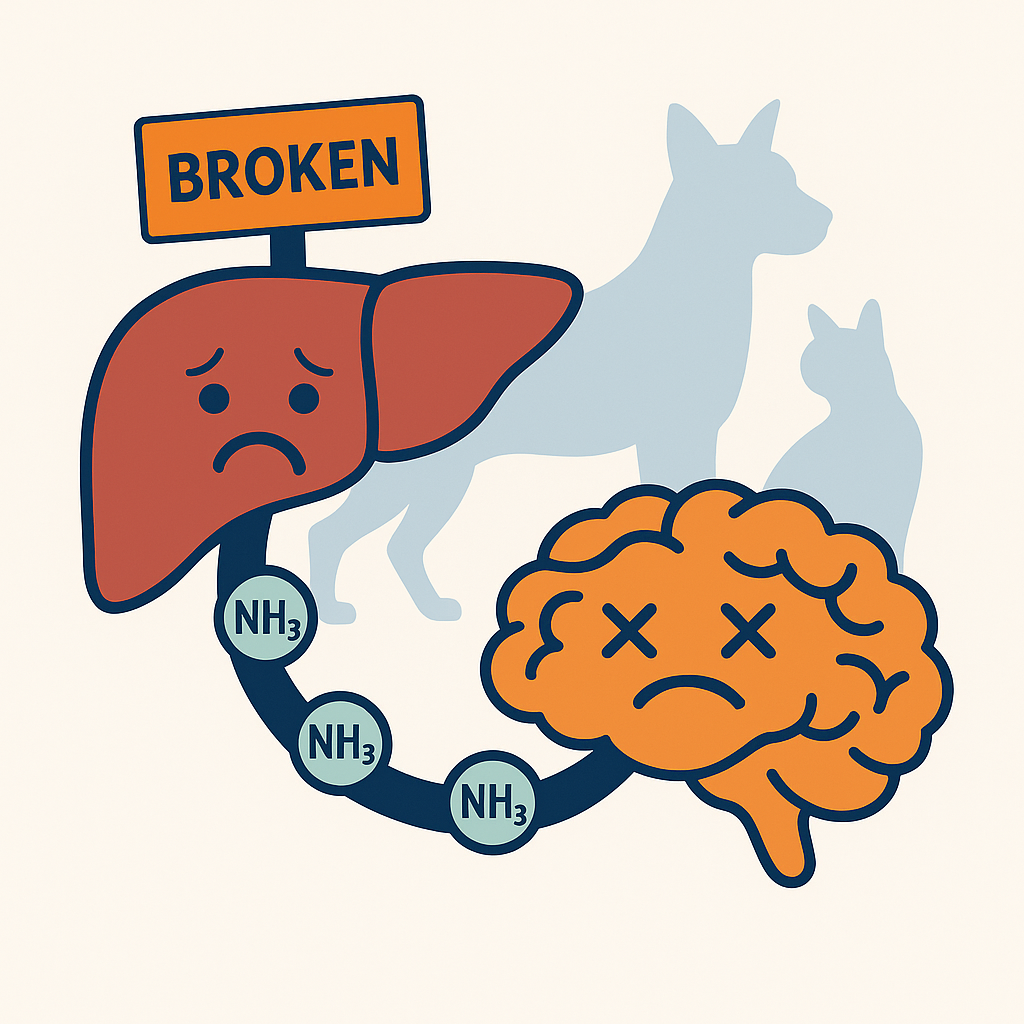
Hepatic encephalopathy (HE) is a serious neurological condition seen in pets with significant liver dysfunction. It develops when more than 70% of liver function is lost, allowing toxins and metabolic byproducts to affect the brain. While the condition is complex, understanding its signs, causes, and treatment options can help both pet parents and veterinary professionals recognize and respond promptly.
What is Hepatic Encephalopathy?
Hepatic encephalopathy is a neurologic syndrome caused by biochemical changes in the body when the liver cannot properly filter toxins. Instead of being detoxified, harmful compounds, such as ammonia, enter the bloodstream and disrupt brain metabolism.
There are three main types of hepatic encephalopathy in pets:
- Type A: Linked to acute liver failure
- Type B: Caused by a portosystemic shunt (abnormal blood vessel) bypassing the liver
- Type C: Associated with chronic liver disease and portal hypertension
Causes and Mechanisms
Several factors contribute to the development of HE, including:
- Ammonia buildup (hyperammonemia): Extra ammonia alters brain chemistry, causing swelling in nerve cells.
- Inflammation: Immune system messengers interfere with brain function.
- Manganese accumulation: Alters brain metabolism and neurotransmission.
- Neurotransmitter imbalances: Elevated serotonin, GABA, and false neurotransmitters disrupt normal nerve signaling.
- Gut microbiota changes: The intestinal bacteria play a large role in ammonia production and neurotransmitter alterations.
Clinical Signs in Pets
Hepatic encephalopathy often presents with a mix of general illness signs and neurological changes.
General signs may include:
- Loss of appetite or nausea
- Diarrhea
- Weight loss
- Lethargy
- Increased drinking and urination
Neurologic signs may include:
- Behavior changes (confusion, aggression, compulsive pacing)
- Head pressing against walls or objects
- Tremors or seizures
- Blindness or deafness
- Stupor or coma in severe cases
Veterinarians grade HE from Grade 0 (no symptoms) to Grade IV (coma or seizures).
Treatment Approaches
Management focuses on reducing toxins, supporting the brain, and treating the underlying liver disease.
Emergency Treatments:
- IV mannitol or hypertonic saline to reduce brain swelling
- Anticonvulsants like levetiracetam for seizures
- Flumazenil to counteract benzodiazepine-like substances
Dietary Management:
- Avoid long-term protein restriction (it can worsen muscle loss and ascites)
- Feed high-quality, easily digestible protein
- Offer frequent, small meals
- Consider diets low in manganese and copper with added zinc
Long-Term Therapies:
- Lactulose: Helps trap and remove ammonia through stool
- Antibiotics (neomycin, metronidazole, amoxicillin): Reduce harmful gut bacteria
- Probiotics: Improve gut health and ammonia breakdown
- Supplements: Zinc, manganese chelators, or L-ornithine L-aspartate (LOLA) in select cases
Prognosis
The outlook depends on the cause and severity. Pets with surgically correctable shunts often do well after treatment. However, those with acute liver failure or advanced chronic disease face a more guarded prognosis. Key negative factors include:
- Severe jaundice (hyperbilirubinemia)
- Prolonged clotting times
- Viral hepatitis or drug-induced liver injury
- Very young or very old age
If neurological signs don’t improve within 72 hours of treatment, further testing for ongoing underlying triggers is recommended.
Key Takeaways for Pet Owners
Work closely with your veterinarian or veterinary specialist to tailor treatment to your pet’s needs.
Hepatic encephalopathy is a serious but manageable condition.
Early recognition of neurological signs in pets with known liver disease is critical.
Specialized diets, medications, and in some cases surgery can significantly improve quality of life.