A common reason for which cats are referred to me is hypercalcemia or elevated blood calcium. Sometimes affected patients are incredibly sick while others have no outward clinical signs of illness. An accurate diagnosis of the underlying cause is truly important. This week I review the major causes of hypercalcemia in cats, and I hope you find the information helpful. Happy reading!

What causes hypercalcemia?
There are multiple potential causes of hypercalcemia in cats. A thorough diagnostic investigation is needed. Idiopathic hypercalcemia (aka no identifiably underlying cause) and cancers are the top causes. While any cancer may theoretically cause elevated blood calcium levels, certain ones are over-represented, particularly lymphoma, multiple myeloma, and squamous cell carcinoma.

Other major possible causes include:
- Kidney disease: Any metabolic insult or toxin that acutely damages the kidneys can cause high blood calcium. A common example is ingestion of ethylene glycol, more commonly known as anti-freeze. Additionally some patients with chronic kidney disease develop elevated blood calcium levels.
- Hyperparathyroidism: The parathyroid glands are located in the neck, and are responsible for helping regulate calcium and phosphorus balance in the body. When these glands secrete too much parathyroid hormone, blood calcium levels often rise and blood phosphorus levels tend to decrease.
- Hypoadrenocorticism: Also known as Addison’s disease, this disorder of the adrenal glands is often associated with high blood calcium levels. Addison’s disease is exceedingly rare in cats.
- Ingestion of excess vitamin D: Certain vitamins and human medications (e.g.: psoriasis ointments) contain vitamin D. When vitamin D is ingested in excess, blood calcium levels can be affected due to the complex relationship between the two in the body.
- Bone destruction: The major mineral component of bones is calcium. Any disease process that causes meaningful damage to bone can cause the release of extra calcium into the bloodstream.
- Fungal infections: In certain parts of the USA, infections caused by fungi readily cause hypercalcemia. These fungal infections include blastomycosis, histoplasmosis, and coccidioidomycosis (also known as Valley Fever).
- Dehydration: When cats don’t drink enough water, they can become dehydrated quickly, a finding that can be associated with mild elevations of total blood calcium.
How is it diagnosed?
The initial documentation of high blood calcium is relatively straightforward. After performing a complete physical examination, a veterinarian will order a non-invasive blood test called a serum biochemical profile. This test measures a form of calcium in the blood called total calcium (tCa). I am advocate for documenting a persistence of hypercalcemia with follow-up testing; simply I recommend evaluating a second fresh blood sample to ensure the abnormality is repeatable before pursuing more extensive testing.
If a total blood calcium level is persistently elevated, then further diagnostic investigation is warranted. Remember one of the most common causes of hypercalcemia in cats is cancer, so I advocate for being as proactive as possible. Partnering with a board-certified veterinary internal medicine specialist can be invaluable for developing an efficient and cost-effective plan for determining the cause of a cat’s high blood calcium level.

A veterinarian will invariably ask you a myriad of questions about your cat’s medical past, including travel history, current medications, and diet. As always, it is exceedingly vital you provide truthful and comprehensive answers to these important questions to help ensure your cat is diagnosed accurately.
Tests that may be recommended include:
- Measurement of ionized blood calcium: Ionized calcium (iCa) is different from total calcium in that the former is considered the active form of calcium in the body. Ionized calcium is involved in various metabolic processes. Total and ionized blood calcium levels can change differently depending on the underlying disease process.
- Diagnostic imaging: Obtaining radiographs/x-rays of the chest and bones, as well as performing sonography of the abdomen, should be recommended for patients with persistently elevated blood calcium levels in an effort to look for evidence of cancerous processes and/or bone damage.
- Measurement of parathyroid hormone related peptide: This unique blood protein, often abbreviated PTHrp, is elevated in many patients living with cancer, specifically lymphoma.
- Measurement of blood vitamin D levels: A finding of an elevated blood vitamin D level should prompt investigation for possible sources of excess exposure to this vitamin.
- Blood & urine kidney values: Kidney function may be evaluated to screen for evidence of renal injury.
- Measurement of parathyroid hormone: Parathyroid hormone (PTH) level is often elevated (or at least inappropriately normal) in patients living with primary hyperparathyroidism.
- Screening for fungal infections: If you live in a part of the world where fungal infections are common, a veterinarian may recommend simple blood and urine tests to screen for certain fungal organisms.
- Testing for Addison’s disease: A simple blood test called an ACTH stimulation test can be performed to definitively screen a patient for Addison’s disease.
How do you treat hypercalcemia?
Effective treatment of hypercalcemia is entirely dependent on the actual cause of a cat’s high blood calcium level. For this reason, a thorough diagnostic investigation is invariably necessary. The treatment for lymphoma is entirely different than the treatment for hyperparathyroidism. Similarly therapy for a fungal infection is vastly different than that for kidney injury. Consulting with a board-certified veterinary internal medicine specialist can be particularly helpful when trying to determine the best way to treat a dog with hypercalcemia.
For cats with idiopathic hypercalcemia, potentially helpful therapies include:
- Dietary manipulation – feeding diets that are fortified with fiber, as well as those that are kidney-friendly and/or designed to help prevent urinary bladder / kidney stone formation, can be helpful in reducing elevated blood calcium levels. Feeding canned diets that are high in protein (40-60%), low in carbohydrates (<15%), and without acidifiers or magnesium restriction may also be effective.
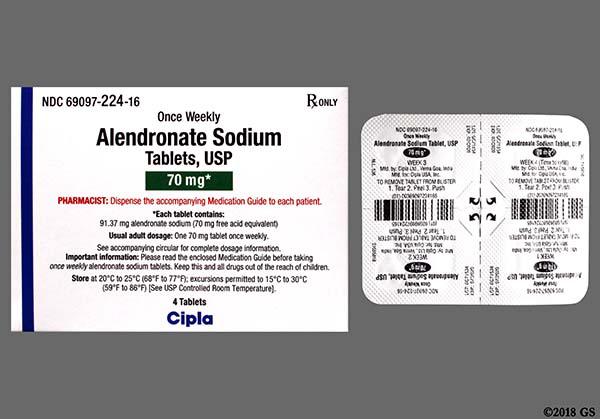
- Bisphosphanate therapy – this class of medication inhibits bone resorption
- Subcutaneous fluid therapy – administration of 0.9% sodium chloride under the skin may help promote the excretion of calcium in urine
- Corticosteroids – this class of steroid reduces both bone resorption and intestinal calcium absorption, as well as increases excretion of calcium by the kidneys
The take-away message about hypercalcemia in cats…
Hypercalcemia or elevated blood calcium is relatively common in cats. The most common causes are idiopathic hypercalcemia and cancers. However other possibilities exist, necessitating a thorough diagnostic investigation. Working with both your family veterinarian and a board-certified veterinary internal medicine specialist is often helpful for progressing through the diagnostic and therapeutic processes efficiently and in a financially responsible manner.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
CriticalCareDVM







