Anyone who has gone to their own doctor knows blood pressure measurement is routine practice. This is because high blood pressure or hypertension is relatively common and can lead to serious issues if not treated appropriately. Well, the same is true of our cats and dogs. Hypertension is a very important issue in our pets, so this week’s post addresses this topic. I hope you find it insightful and shareworthy. Happy reading!
What is hypertension?
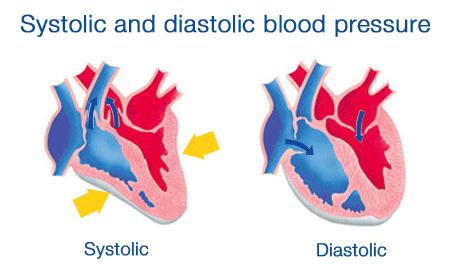
In humans, blood pressure is recorded as two numbers:
- Systolic blood pressure (the first number) – this value indicates how much pressure your blood is exerting against artery walls when the heart beats
- Diastolic blood pressure (the second number) – this values tells us how much pressure your blood is exerting against artery walls while the heart is resting between beats.
Due to challenges in measuring blood pressure in cats and dogs versus humans, veterinarians pay more attention to systolic blood pressure in pets. Systemic hypertension is defined as a sustained increase in systolic blood pressure ≥140 mmHg.
There are three recognized categories of systemic hypertension: situational, secondary, and idiopathic.
- Situational hypertension: This form is the result of excitement, fear, and/or anxiety associated with the process of blood pressure measurement in a patient who otherwise has a normal blood pressure. Some patients experience situational hypertension while others do not. This type of hypertension resolves with a reduction or elimination of the physiologic stimulus.
- Secondary hypertension: This form is defined as a persistently increased blood pressure due to a disease known to cause hypertension, the administration of a drug known to elevated blood pressure, and/or a toxin that induces hypertension. Secondary hypertension is the most common cause of hypertension in cats and dogs.
- Idiopathic hypertension: This form of hypertension occurs without an overt underlying cause. Often referred to as primary or essential hypertension in people, idiopathic hypertension is relatively uncommon in cats and dogs.
Hypertension is further categorized based on risk of inducing organ damage:
- Prehypertension: 140-159 mmHg
- Hypertension: 160-179 mmHg
- Severe hypertension: ≥180 mmHg
What causes it?
Diseases that cause elevations in cardiac output, systemic vascular resistance, heart rate, and/or stroke volume can cause systemic hypertension. Blood pressure is regulated by interactions between a variety of chemicals in the body (e.g.: catecholamines, renin-angiotensin-aldosterone system, prostaglandins, atrial natriuretic peptide, vasopressin), central nervous system, peripheral nervous system, the heart, and kidneys.
There are several diseases with which dogs and cats may be diagnosed that may cause hypertension, including:
- Kidney diseases
- Hyperadrenocorticism (Cushing’s disease)
- Diabetes in cats & dogs
- Obesity
- Hyperaldosteronemia
- Pheochromocytoma
- Hyperthyroidism
- Hypothyroidism
- Brachycephalic conformation
What does hypertension look like?
There is no breed, age, or sex predilection for situational or idiopathic hypertension. Patients with secondary hypertension are most commonly presented by their families for clinical signs associated with a primary condition that causes high blood pressure. For example:
- Chronic kidney disease – weight loss, increased thirst and/or frequency of urination, inability to hold head up, reduced (or loss of) appetite, constipation
- Hyperadrenocorticism (Cushing’s disease) – increased panting, increased thirst and/or frequency of urination, weakness, weight gain, recurrent skin and/or urinary tract infections
- Diabetes mellitus – increased thirst and/or frequency of urination, weight loss, increased appetite, cataracts, urinary tract infections
- Hyperaldosteronemia – inability to hold head up, hind limb weakness, difficulty jumping, lethargy, listlessness, unsteadiness while walking (called ataxia)
- Pheochromocytoma – weakness, collapse, lethargy, reduced (or loss of) appetite, vomiting, panting, weight loss, anxiety, restlessness, increased thirst and/or frequency of urination, diarrhea, abdominal distension, hind limb swelling, epistaxis (nose bleeding), seizures, vision loss
- Hyperthyroidism – increased thirst and/or frequency of urination, weight loss, increased appetite, unkempt hair, restlessness, aggression, increased respiratory rate, increased vocalization, heat avoidance
- Hypothyroidism – reduced activity level, weight gain, chronic skin and/or ear infections, excessive shedding, facial drooping, heat-seeking behavior, regurgitation
Hypertension may cause meaningful damage to several organs in the body (called target organ damage), including:
- Kidneys – may cause elevated blood kidney values and/or excess loss of protein in the urine
- Eyes – may cause bleeding in different parts of the eye, increased pressure in the eye (called glaucoma), and acute blindness
- Brain – may cause a variety of neurological deficits
- Heart – may cause abnormal heart sounds and rhythms, as well as changes to size of the heart
- Vasculature (blood supply) – may lead to epistaxis (nose bleeding) and/or stroke events
How is it diagnosed?
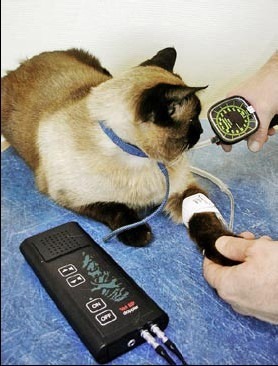
Blood pressure may be measured via two general methods: direct measurement and indirect measurement. To directly measure blood pressure, a veterinarian places a catheter directly into an artery in a leg. The catheter is then connected to a specialized monitor that provides a blood pressure measurement. Direct blood pressure monitoring is not routinely performed in primary care hospitals but is common in referral settings. In contrast, blood pressure is most commonly measured indirectly in dogs and cats by placing a special cuff around a limb over an artery. The two indirect monitoring methods are the use of a Doppler machine and the use of an oscillometer.
If a patient is found to be living with hypertension, then a subsequent diagnostic investigation may be needed to determine the underlying reason for the elevated blood pressure. Pet owners may find it helpful to collaborate with a board-certified veterinary internal medicine specialist to develop a logical and cost-effective diagnostic plan.
How is hypertension treated?
Situational hypertension does not require intervention. Antihypertensive therapy should be initiated for any patient with documented hypertension and suspected/confirmed target organ damage. Furthermore, concurrent therapy for any primary condition causally associated with secondary hypertension is indicated.
Veterinarians will tailor treatment to decrease the likelihood and severity of target organ damage. The goal of therapy is to achieve a systolic blood pressure <140 mmHg. Pet owners may find it helpful to partner with a board-certified veterinary internal medicine specialist to develop an effective treatment plan.
The take-away message about hypertension in cats & dogs…
Hypertension is a common medical issue in cats and dogs. High blood pressure is most commonly a problem induced by another health condition. As such, both a thorough diagnostic investigation and appropriate interventions are needed to prevent target organ damage. Routine annual screening for systemic hypertension is recommended in older patients.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
CriticalCareDVM