I’ve previously published information about diabetes mellitus in dogs, including details about how to treat this disease. What if a dog or cat had too much insulin instead of too little? This is a serious condition called insulinoma. This week I’ve dedicated time to sharing some helpful tidbits about this problem. Happy reading!
Insulinoma – What is it?
The pancreas produces and secretes hormones that facilitate carbohydrate metabolism. The Islets of Langerhans, also called pancreatic islets, contains five distinct cells types, each with its own hormone product:
- Alpha cells – produce glucagon (~20% of total islet cells)
- Beta cells – produce insulin and amylin (~70% of total islet cells)
- Delta cells – produce somatostatin (<10% of total islet cells)
- Gamma (or PP) cells – produce pancreatic polypeptide (<5% of total islet cells)
- Epsilon cells – produce ghrelin
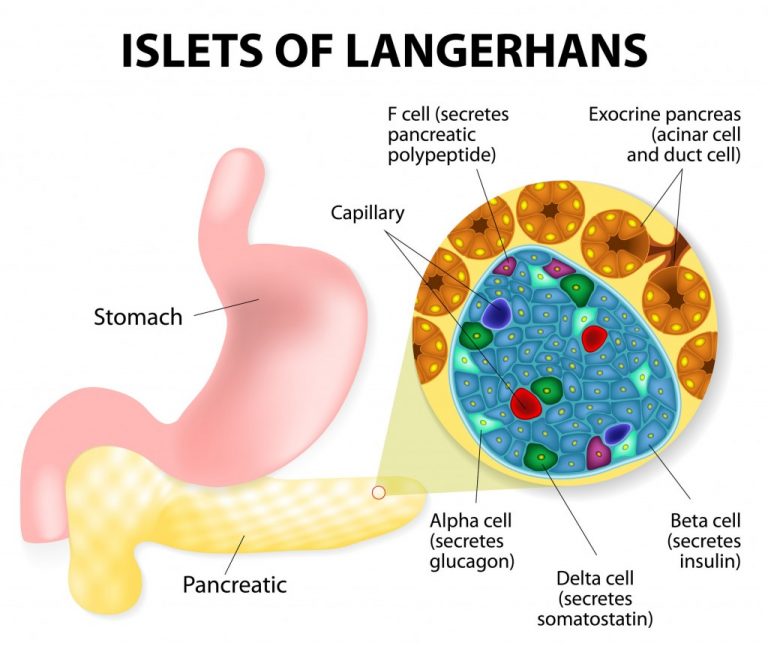
Insulin is secreted by beta cells in the pancreatic islets in response to hyperglycemia (high blood sugar). Dogs maintain euglycemia (normal blood sugar) even with fasting under normal circumstances. Insulinoma is most commonly a cancerous tumor of beta cells in pancreatic islets characterized by inappropriate insulin secretion and subsequent (and often marked) hypoglycemia (low blood sugar). The mechanism by which autonomous insulin secretion occurs is not yet known.
Insulinoma – What does it look like?
Dogs with insulinoma are typically middle-aged or geriatric (median age: 10 years). There is no breed or sex predilection. Typical patient histories indicate affected dogs have had clinical signs for 1-6 months, although some studies have reported duration of clinical signs up to three years. Clinical signs associated with hypoglycemia include:
- Lethargy
- Confusion & disorientation
- Weakness
- Ataxia (unsteadiness while walking)
- Seizures
- Restlessness & nervousness
- Muscle tremors
- Increased thirst
- Increased frequency of urination
- Increased hunger
Whipple’s triad is the term used to describe three criteria that, when satisfied, confirm a patient’s clinical signs are due to hypoglycemia:
- Clinical signs consistent with hypoglycemia
- Documented hypoglycemia
- Resolution of clinical signs with increasing blood glucose concentration
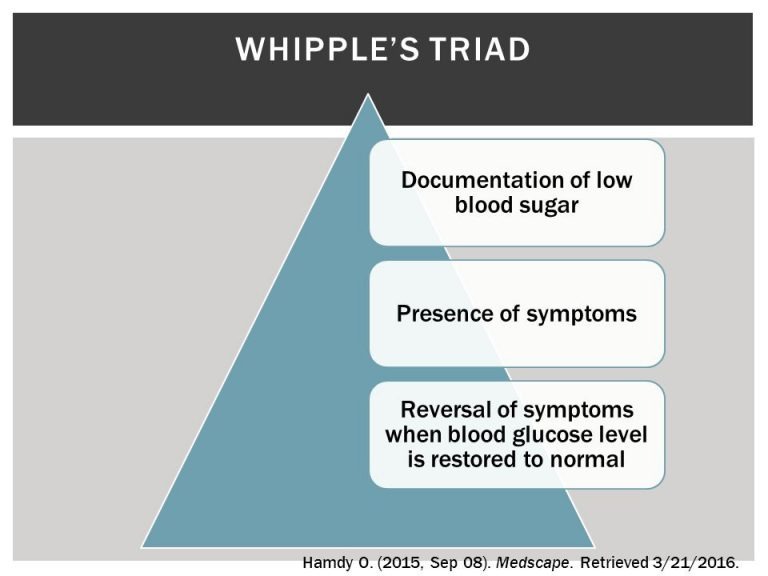
The onset and severity of clinical signs depends on the degree of hypoglycemia and the rate at which serum glucose concentration decreases. Interestingly, some dogs don’t have any clinical signs despite marked hypoglycemia because they adapted over a prolonged period. In dogs with insulinoma, serum glucose concentration declines rapidly with fasting, exercise, and/or excitement. Rebound hypoglycemia 1-6 hours after a meal is also possible since the initial rise in blood sugar triggers enhanced insulin secretion.
Insulinoma – How is it diagnosed?
A veterinarian must perform a properly through diagnostic investigation to rule out other possible causes of low blood sugar, including:
- Acute liver failure
- Hypoadrenocorticism (Addison’s disease)
- Sepsis
- Inappropriate insulin administration
- Absolute polycythemia
An insulinoma is presumptively diagnosed based on hypoglycemia, hyperinsulinemia (elevated blood insulin level), and appropriate clinical signs. Finding an insulinoma, however, is not always a straightforward process. A veterinarian may recommend various imaging modalities to identify this cancerous process:
- Abdominal Radiography (x-rays) – Radiography is clinically useless for identifying insulinoma. However, this modality is helpful for ruling out some of the other causes of hypoglycemia.
- Chest Radiography – Chest radiography should be performed in all patients suspected of living with insulinoma to screen for evidence of cancerous spread to the thoracic cavity.
- Abdominal Sonography – Use of sonography is one of the most common diagnostic imaging modalities used to identify insulinoma. Unfortunately, in most studies to date pancreatic lesions were identified in less than 50% of dogs within insulinoma.
- Abdominal Computed Tomography (CT) – Insulinoma are slightly hypodense (darker grey) compared with liver tissue. Density increases uniformly or irregularly after contrast enhancement, but remains hypodense compared to liver tissue.
- Scintigraphy – Administration of medical grade radioactive chemical may be useful for identifying some pancreatic lesions.
Other tests that may be performed in patients suspected of living with insulinoma are serum fructosamine and amended insulin to glucose ratio (AIGR). Definitive diagnosis required biopsy confirmation. Pet parents will likely find it helpful to consult with a board-certified veterinary internal medicine to develop a logical and cost-effective diagnostic plan.
Insulinoma – How is it treated?
Clinical signs associated with hypoglycemia should be controlled prior to surgery. Surgery allows definitive diagnosis. Pancreatic surgery is quite intricate, and pet parents are strongly encouraged to partner with a board-certified veterinary surgeon. Survival time is improved when a solitary nodule is removed. Furthermore, debulking metastatic lesions tends to improve clinical signs and response to medical management. Unfortunately, some pancreatic tumors can’t be identified. When this happens, a common recommendation is to remove ~50% of the pancreas in hopes of removing the cancerous tumor. Acute pancreatitis and persistent hypoglycemia are the most common potential post-operative complications. The latter is a negative prognostic factor as it implies persistent cancerous tissue.

Chronic medical management is indicated for patients who are not surgical candidates, those whose families decline surgery, and those with persistent post-operative hypoglycemia. The goals of medical management are not establishing and maintaining euglycemia. Rather, the goal is resolution of clinical signs associated low blood sugar. Medical interventions include:
- Dietary manipulation – Feeding small frequent meals composed of complex carbohydrates, as well as high levels of fat and protein, reduce the incidence of insulin spikes after meals.
- Exercise – In general, physical activity level should be limited whenever possible. Short periods of low-impact exercise aren’t often associated with worsening of hypoglycemia.
- Steroids – Steroid stimulate the liver to form new sources of blood sugar.
- Diazoxide – This drug inhibits insulin secretion and stimulates the liver to form new sources of blood sugar.
- Octreotide – Octreotide inhibits insulin release from pancreatic beta cells.
- Streptozotocin – This is a potent intravenous chemotherapeutic agent that directly damages beta cells. Potential adverse effects include vomiting, liver enzyme changes, and diabetes mellitus.
- Tyrosine kinase inhibitors – Research in humans with pancreatic tumors suggested potential benefit of treatment with tyrosine kinase inhibitors. Although there is no published research in dogs with insulinoma, anecdotal evidence regarding efficacy exists. Potential adverse effects are diarrhea, nausea/vomiting, hyporexia/anorexia, myelosuppression, and proteinuria.
Insulinoma is classified as follows:
- Stage I – insulinoma confined to the pancreas
- Stage II – insulinoma with regional lymph node metastasis
- Stage III – insulinoma with distant metastasis
Research has shown median survival times (MST) of 785 days, 547 days, and 217 days for Stage I, Stage II, and Stage III, respectively. This group also showed longer MST with surgical management compared to medical management (785 days vs. 196 days).
The take-away message about insulinoma in dogs…
Insulinoma is a cancer of pancreatic beta cells characterized by excess secretion of insulin. Too much insulin causes blood sugar to drop to very low levels. Clinical signs are often variable. Early identification is of paramount importance. Surgery followed by medical management is associated with the best outcomes.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
To find a board-certified veterinary cancer specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
CriticalCareDVM





