Some of the most commonly measured blood values in dogs and cats are liver enzymes. When elevations occur, one may logically assume an elevation of a specific liver enzyme means the problem lies with the liver itself. But that isn’t always the case, and in this week’s post, I share some information about liver enzymes and why their blood levels rise. Happy reading!
Liver enzymes – What are they and why do they elevate?
One of the non-invasive blood tests veterinarians frequently perform in both during sickness and as part of a preventative healthcare screening is called a serum biochemical profile (often simply referred to as a CHEM). Liver enzyme measurement is a standard component of a CHEM, and these enzymes can be classified into two groups:
Hepatocellular enzymes
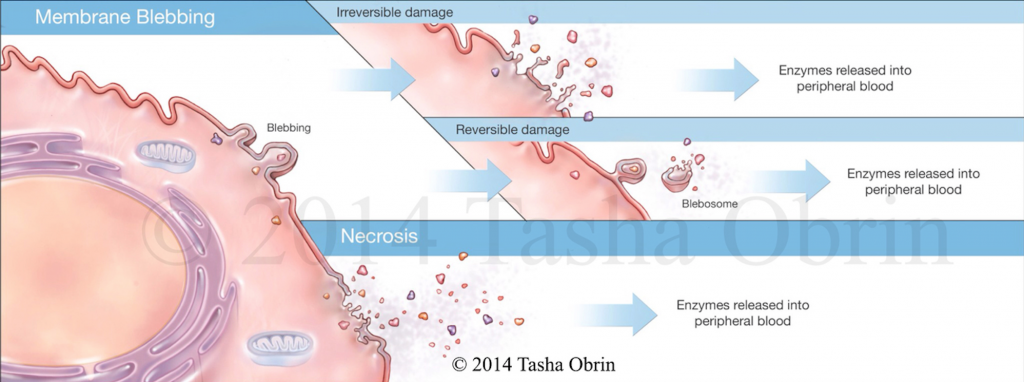
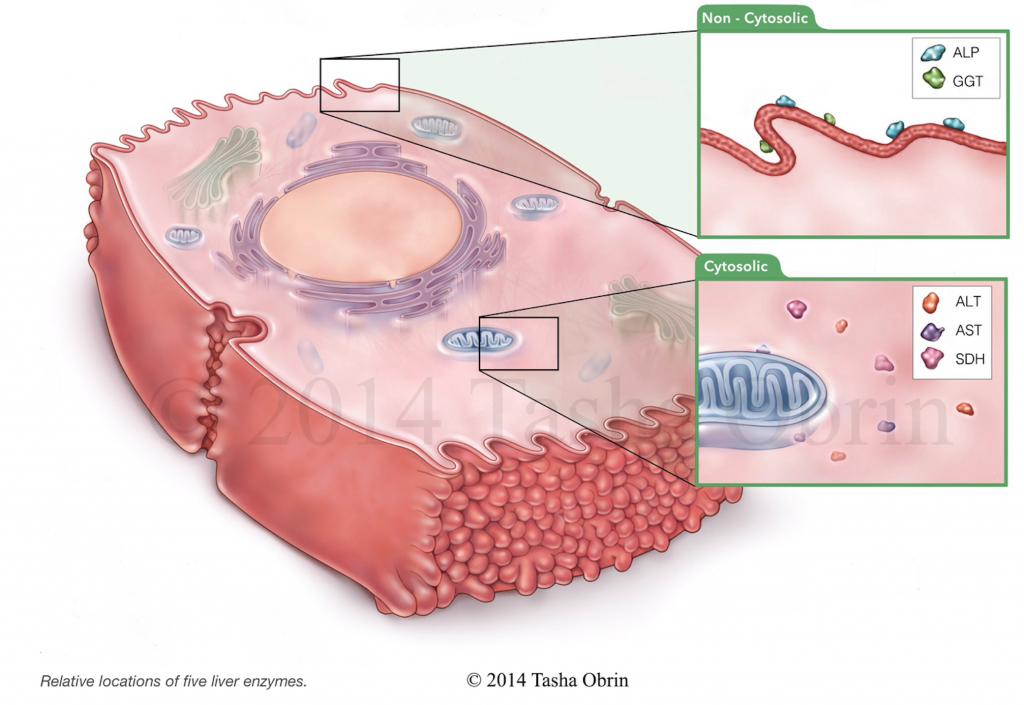
- Alanine aminotransferase (ALT; also called glutamic pyruvate transaminase/SGPT): This enzyme is found inside all individual liver cells and, to a lesser extent, inside skeletal muscle cells. ALT enters the bloodstream when liver cell membranes are damaged or individual liver cells die (called necrosis), allowing it to leak into the blood.
- Aspartate aminotransferase (AST; also called glutamic oxaloacetic transaminase/SGOT): Similar to ALT/SGPT, this enzyme is also found inside all individual liver cells. However it is also found a skeletal muscle, heart muscle, and the kidneys. When liver cell membranes are damaged or liver cells breakdown, this enzyme leaks into the bloodstream.
Cholestatic enzymes
- Alkaline phosphatase (ALP): This enzyme is found in many organs throughout the body, including bone and intestinal tract; in the liver it is made in cells that line bile ducts. When there is an obstruction to proper bile flow through the liver, this enzyme becomes elevated in the bloodstream.
- Gamma glutamyl transferase (GGT): This is another enzyme found in multiple organs throughout the body, including small intestines, kidneys and pancreas. In the liver GGT is found in the cell membranes of bile ducts, and when elevated, veterinarians worry about diseases that impede the flow of bile.
Liver enzymes – How else do veterinarians evaluate the liver?
There are a few additional blood and urine values veterinarians may perform to help decide if the liver, itself, is the reason for liver enzyme elevations. Some of these are routinely measured as part of a CHEM while veterinarians order others only after a review of a CHEM raises further suspicion for abnormal liver function.
Below are some blood and urine values that give veterinarians indirect evidence about liver function:
- Bilirubin: Bilirubin is predominantly the breakdown product of hemoglobin, the major oxygen carrying protein in the body. The liver is responsible for metabolizing it appropriately, and liver dysfunction is a major reason blood bilirubin levels rise.
- Albumin: As I discussed in a recent post, albumin is the body’s major protein that is made by the liver. When 60-80% of liver function is lost, the albumin level in blood drops.
- Blood glucose (GLU or BG): Glucose is absorbed from the gastrointestinal tract after digestion of food, and circulates in blood to the liver where it is converted to a molecule called glycogen. Glucose can also be made in the liver during a process called gluconeogenesis. When liver function is abnormal, the liver’s ability to convert glucose to glycogen, as well as the ability to perform gluconeogenesis, is often compromised.
- Cholesterol (CHOL): The liver is the major site of cholesterol production. When the liver is not functioning appropriately, blood cholesterol concentrations decrease.
- Blood urea nitrogen (BUN): Ammonia delivered from the gastrointestinal tract is converted to BUN. When liver function is abnormal, BUN levels decrease and blood ammonia levels increase.
- Blood coagulation/clotting factors: Many proteins that prevent the body from spontaneously bleeding are made in the liver. With meaningful liver dysfunction, these blood coagulation factors are not adequately synthesized, and measurement of the body’s clotting times are often prolonged.
- Urine bile acids: An abnormal result is strong evidence of for liver dysfunction.
- Urine ammonium urate/biurate crystals: These crystals can occasionally be found in patients with liver shunts and severe liver disease. Ammonia is made in the gastrointestinal tract and subsequently transported to the liver to be metabolized. A major component of this metabolism is conversion of ammonia to BUN. With liver dysfunction blood ammonia levels rise, and the metabolism of another metabolic by-product called uric acid is disrupted. Thus ammonia and uric acid combine to form ammonium urate and biurate crystals. Furthermore these crystals can stick to each other to form large conglomerations called uroliths (bladder stones).

Below are some non-invasive blood tests that give direct evidence of liver dysfunction:
- Serum bile acids (SBA): Bile acids are made in individual liver cells and subsequently secreted into bile ducts. The bile acids are circulated in the digestive tract to help breakdown certain types of foods, and are then reabsorbed through the gastrointestinal tract and into liver cells to be used again. Elevated SBA values are relatively specific for detecting abnormal liver function caused by either abnormal liver blood flow (called portal circulation), disrupted reabsorption by liver cells, and/or reduced secretion into the biliary system.

- Ammonia: As a result of normal metabolism, ammonia is produced in the gastrointestinal tract. It is subsequently absorbed into the bloodstream and circulated to the liver where it is removed by that organ.
Liver enzymes – What if the liver really is the problem?
After reviewing a complete patient history, performing a thorough physical examination, and reviewing the results of blood/urine tests (like those listed above), a veterinarian will determine if additional testing is indicated to further investigate the liver’s role in causing liver enzyme elevations. Additional assessments that may be recommended include diagnostic imaging (i.e.: abdominal radiography/x-rays +/- abdominal ultrasonography, scintigraphy, computed tomography/CT scan) and liver biopsies. There are several methods by which one may obtain a liver biopsy from dogs and cats. Consultation with a board-certified veterinary internal medicine specialist and/or a board-certified veterinary surgeon is often invaluable to develop a logical and cost-effective diagnostic strategy for a pet at this point.
Liver enzymes – What if the liver isn’t the problem?
Cumulative testing as described above may ultimately tell your veterinarian that liver dysfunction is not the reason your pet’s liver enzymes are elevated. Some relatively common causes of liver enzyme elevations that are not primarily the liver’s fault, include:
- Hyperadrenocorticism (Cushing’s disease) – a state of over-functioning of part of the adrenal gland called the cortex
- Pancreatitis – inflammation of the pancreas
- Hypothyroidism – a state of under-functioning of the thyroid gland
- Hypoadrenocorticism (Addison’s disease) – a state of under-functioning of the adrenal cortex
- Drug induction – some medications, particularly steroids, can cause certain liver enzymes to increase
- Primary gastrointestinal disease – when the gastrointestinal tract is disease (i.e.: inflammatory bowel disease, cancer), certain inflammatory chemicals are released and circulate to the liver to cause liver enzyme elevations
- Gallbladder disease – some patients develop gallstones (called choleliths) and/or thick conglomerations of mucus and bile in the gallbladder (called a mucocele) that disrupt bile flow and cause some liver enzymes to elevate
- Certain cancers – various malignant processes can cause elevations in certain liver enzymes
The take-away message about liver enzymes…
Liver enzymes can be confusing because abnormal values don’t necessarily mean there’s a problem with the liver. Some simple non-invasive blood and urine tests can be performed to shed helpful light on this issue, and consultation with a board-certified veterinary internal medicine specialist is frequently uniquely helpful to get to the bottom of the problem efficiently and cost-effectively.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
Wishing you wet-nosed kisses,
cgb


Great article and images! I just wanted to note that ALKP enzymes are only cortisol induced in the dog. So, they can be elevated in stress, hyperadrenocorticism, or steroid administration in the dog, but not the cat.