Chronic coughing is a frequent health concern of dog parents. In a previous blog, I discussed the most common cause of this sign in dogs – chronic bronchitis. Another reason for dogs to cough habitually is tracheal collapse (e.g. collapsing trachea). This week I discuss this common condition, and hope you find the information helpful. Happy reading!
Tracheal Collapse – What is it?
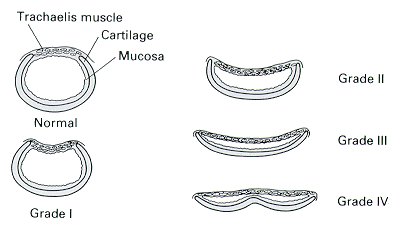
The trachea of dogs, also called the windpipe, is a long flexible tube of cartilage and muscle that connects the mouth to the lower airways of the lungs (e.g. bronchi). Part of the trachea is in the neck (called the cervical trachea), and another part is inside the chest cavity (called the thoracic trachea). The transition point from neck to chest cavity is called the thoracic inlet. The cartilage is C-shaped with the open part facing upward. In some dogs, this cartilage weakens and flattens, resulting in collapse of the trachea and causing airway compromise. The most common point of collapse is at the level of the thoracic inlet, and the degree of collapse is variable. Veterinarians grade tracheal collapse as follows:
- Grade I – 25% collapse
- Grade II – 50% collapse
- Grade III – 75% collapse
- Grade IV – 100% collapse
Occasionally some of the lower airways, specifically the bronchi, concurrently collapse with the trachea. Tracheal collapse may occur in any dog, but some breeds are over-represented:
- Yorkshire Terriers
- Chihuahuas
- Pomeranians
- Miniature Poodles
In the video below, one can see the dynamic changes that occur in patients with tracheal collapse. During inspiration (breathing in), the cervical trachea collapses. During exhalation (breathing out), the thoracic trachea collapses.
Clinical signs frequently associated with tracheal collapse include:
- A dry, non-productive cough that sounds like a goose honk
- Coughing with excitement, when picked up, and/or when pressure is applied to the neck
- Exercise intolerance
- A click-like noise heard when exhaling (breathing out)
- Difficulty breathing
- Fainting / collapse
- Wheezing when inhaling (breathing in)
Tracheal collapse is typically documented in middle aged to older dogs, but young patients may be affected too. Overweight and obese dogs, as well as those exposed to secondhand smoke, seem more likely to show clinical signs.
Tracheal Collapse – How is it diagnosed?
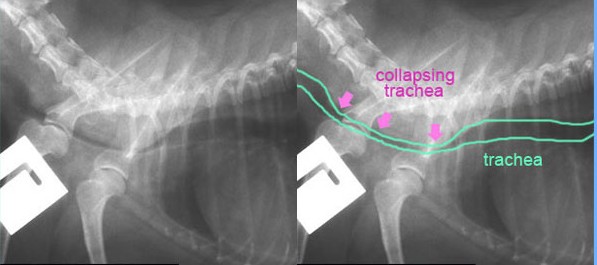
Your family veterinarian will recommend some non-invasive or minimally invasive tests to diagnose the degree of tracheal collapse. Initially chest radiographs (x-rays) are obtained in an attempt to make a definitive diagnosis, as well as to screen for other potential causes of chronic coughing. Pet parents should remember tracheal collapse is fundamentally a dynamic process, and thus the tracheal isn’t always collapsed (except in severe cases). A radiograph is essentially a single picture taken at a specific point in time. If the picture is captured when the trachea is collapsed, then a veterinarian is able to make a definitive diagnosis. However, if the x-ray image is obtained when the tracheal isn’t collapse, radiography will not be fruitful, and additional testing will be necessary.
When radiographs don’t provide a definitive diagnosis of tracheal collapse, your family veterinarian will likely refer you to a board-certified veterinary internal medicine specialist for further testing. Advanced diagnostic imaging will be recommended, potentially including:
- Fluoroscopy – this is a live-action radiograph that is obtained while an awake patient breathes normally. In the video below, one can see tracheal collapse in the neck documented via fluoroscopy.
- Tracheoscopy – this is a minimally-invasive imaging test performed while a patient is anesthetized. A small fiber-optic camera is inserted into the trachea to give the best detail of this tube. Fluids samples can also be easily obtained for analysis during this procedure. In the video below, one can see marked tracheal collapse documented during tracheoscopy.
Tracheal Collapse – How is it treated?
Tracheal collapse is a chronic, progressive, and irreversible condition. Accordingly, it is one that is initially treated medically but with progression will likely require surgical management. The hallmarks of medical management include:
- Medication(s) to reduce frequency and severity of coughing
- Medication(s) to reduce anxiety
- Maintenance of an ideal body weight
- Medication(s) to reduce airway inflammation, mucus production, and spasms
- Avoidance of secondhand smoking and other environmental airway irritants
Some patients with tracheal collapse develop severe respiratory distress, and require emergency veterinary care. Thankfully almost three quarters of tracheal collapse patients will positively respond to medical management, particularly those with grade I and II disease. With time, tracheal collapse progresses and fails to respond to medical interventions. For such patients, surgical management is necessary, and typically involves either placing a stent inside the trachea or placing plastic rings outside of it to hold it open. Approximately 90-95% of patients who receive tracheal stents immediately and markedly improve, while approximately 75% of patients improve after surgical placement of rings.

The take-away message about tracheal collapse in dogs…
The trachea or windpipe in dogs is a tube of cartilage and muscle. Occasionally the cartilages weaken and collapse, resulting in chronic coughing and potentially respiratory distress. A combination of physical examination findings and diagnostic imaging studies is used to confirm a diagnosis of tracheal collapse. Initial treatment is medical in nature, aimed at reducing coughing frequency and severity, reducing airway inflammation, and minimizing anxiety. As tracheal collapse progresses, surgical intervention will be necessary. Partnering with board-certified veterinary internal medicine specialists and board-certified veterinary surgeons can be instrumental in ensuring an efficient diagnostic process and developing an effective treatment plan.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
Wishing you wet-nosed kisses,
cgb





