The heart is a vital organ. It pumps blood throughout the body, delivering oxygen-rich blood to organs and returning oxygen-poor blood back to the lungs to be loaded with oxygen. There are a variety of ailments that cause the heart to function abnormally, impairing its ability to circulate blood. This week I’ve dedicated a post to one of these causes – pericardial effusion. I hope you find the information helpful and insightful! Happy reading!

What is pericardial effusion?
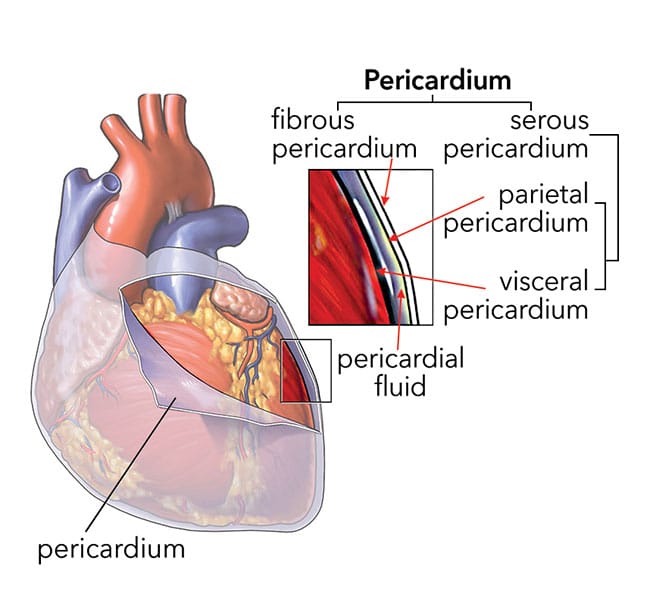
To understand pericardial effusion one needs to have a basic understanding of heart anatomy. The heart is the pump that distributes blood throughout the body. It has four chambers: two atria and two ventricles. Surrounding the heart is a sac called the pericardium. The pericardium has two layers – an outer fibrous layer and an inner serous layer. The serous pericardium is further divided into parietal and visceral layers.
The space between the parietal and serous layers is called the pericardial cavity. This cavity normally contains a very small volume of fluid called plasma ultrafiltrate (1-15 mLs). The pericardium supports the heart and protects from both cancer and a variety of infections.
Pericardial effusion is excess accumulation of fluid in the pericardial cavity. Fluid may accumulate gradually or rapidly depending on the underlying disease process. When too pericardial effusion is present, the pressure inside the pericardial cavity rises. This increased pressure can cause the chambers of the heart to collapse, inhibiting adequate flow of blood through and out of the heart. This scenario is called cardiac tamponade. The lungs, trachea (windpipe), and esophagus (food pipe) may also be compressed, contributing to clinical signs.
Major causes of pericardial effusion include:
- Cancer – the most cancers documented to cause pericardial effusion are hemangiosarcoma, chemodectoma, and mesothelioma. Cancers in other parts of the body can also spread to the pericardial cavity.
- Right-sided heart failure
- Low albumin (major protein of the body)
- Infectious diseases – although not common, both fungal and bacterial infections can cause pericardial effusion
- Idiopathic – this term is used when we can’t identify an underlying cause after a thorough diagnostic investigation
- Cysts – these represent a congenital cause of pericardial effusion
- Peritoneopericardial diaphragmatic hernia – this is a congenital lesion in which the thoracic and abdominal cavities are incompletely separated
What does it look like?
Any dog can develop pericardial effusion, but this condition is most commonly documented in large breed dogs like Golden retrievers and German shepherds. Male dogs appear to be over-represented and median age in 7-9 years. The most common clinical signs noted by families are:
- Weakness & collapse (called syncope)
- Coughing
- Abdominal distension
- Rapid breathing
- Sudden death
How is it diagnosed?
A veterinarian will perform a thorough physical examination. Common abnormalities noted on evaluation include:
- Elevated heart rate
- Distension of the external jugular vein (major vein in the neck region)
- Muffled heart sounds
- Weak & abnormal pulses
- Pale gums
- Prolonged capillary refill time
If a patient’s history and physical examination raise suspicions for pericardial effusion, the doctor will likely perform diagnostic imaging. The best imaging modality is ultrasonography of the heart, as it allows for confirmation of pericardial effusion, assessment for cardiac tamponade, and visualization of any masses within the pericardial cavity. If ultrasonography is not available, radiography (x-rays) can be helpful.
How is it treated?
Pericardial effusion is considered a life-threatening problem, and sudden death is possible. Upon confirmation of this problem, a veterinarian should perform a minimally invasive procedure called a pericardiocentesis. Some veterinarians are not comfortable performing this procedure, and thus you may be referred to a specialty and emergency hospital.
A pericardiocentesis involves guiding a needle & catheter through the chest wall into the pericardial cavity to allow evacuation of the excessive pericardial effusion. Please watch the video below to watch a veterinarian perform a pericardiocentesis.
Patients should receive pain medication – both systemically and locally. Some require sedation. A patient’s heart rhythm is monitoring via electrocardiography (ECG/EKG) throughout the procedure because life-threatening abnormal heart rhythms are possible during pericardiocentesis. The medical team should be prepared to administer medications (i.e.: 2% lidocaine) to correct any noted abnormal heart rhythms. With removal of the excessive pericardial fluid, a patient’s condition usually rapidly improves.
It’s imperative to allow a veterinarian to perform a thorough diagnostic investigation to determine the underlying cause. Without proper identification of the actual cause and subsequent appropriate therapy, a successful outcome may not be possible. Some patients need surgery to remove part of the pericardium and/or to remove a cancerous mass (if possible). The most common types of pericardial surgeries are:
- Partial pericardiectomy performed via median sternotomy or right lateral thoracotomy
- Thoracoscopy pericardiectomy
- Percutaneous balloon pericardiotomy
These are complicated surgeries, and pet parents are strongly encouraged to partner with a board-certified veterinary surgeon.
The take-away message about pericardial effusion in dogs…
Pericardial effusion is excessive accumulation of fluid in the pericardial cavity. Major causes include cancers and right-sided heart failure, although sometimes a cause can’t be identified. Treatment involves removal of the excessive pericardial effusion via a procedure called a pericardial effusion, as well as determining the cause of fluid accumulation.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
Wishing you wet-nosed kisses,
CriticalCareDVM





