Heartburn is an uncomfortable feeling caused by stomach acid splashing into the esophagus. Also called acid reflux, people often take various over-the-counter medications to alleviate discomfort associated with heartburn. Severe and/or chronic acid reflux is called gastroesophageal reflux disease, and may be associated with more serious conditions. Like humans, dogs and cats are affected by GERD, so in this week’s post, I share some information about this potentially painful syndrome. Happy reading!
GERD – What is it?
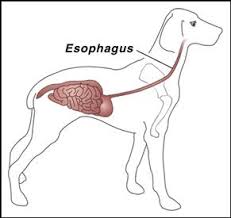
Gastroesophageal reflux disease, commonly referred to as GERD, is a chronic disease that occurs when stomach acid flows back into the food pipe (called the esophagus). This reflux of stomach acid subsequently and chronically irritates the lining of the esophagus (called the mucosa) to cause the clinical signs associated with this syndrome.
GERD – What does it look like?
Recognizing GERD in dogs and cats is not always straightforward. These fur babies can’t tell us they feel a burning sensation in their chests like people can. They can’t tell us about a feeling like they have a lump in their throats. Nevertheless, there are some clinical signs that when present should raise the proverbial red flag of concern. These include:
- Difficulty swallowing (called dysphagia)
- Regurgitation
- Reduced appetite
- Change in the nature of a bark or meow
- Generalized discomfort
- Chronic nasal discharge and/or sneezing
- Chronic non-productive coughing
GERD – How is it diagnosed?
After thoroughly reviewing a patient’s medical history and performing a complete physical examination, a veterinarian will perform some logical diagnostic tests to screen for underlying diseases contributing to GERD. These tests may include:
- Complete blood count – a non-invasive blood test to evaluate white blood cells, red blood cells, and platelets (cells that help the body form proper blood clots)
- Biochemical profile – a non-invasive blood test that that gives information of liver health, kidney function, gastrointestinal enzymes, and electrolytes (e.g. sodium, potassium)
- Urinalysis – a non-invasive urine test to screen for kidney damage, some metabolic conditions, and infection
- Abdominal imaging – radiographs (x-rays) and/or ultrasonography allows the veterinarian to evaluate the organs within the abdominal cavity
- Thoracic/Chest imaging – radiographs of the chest are essential for visualizing the esophagus, lungs, and heart
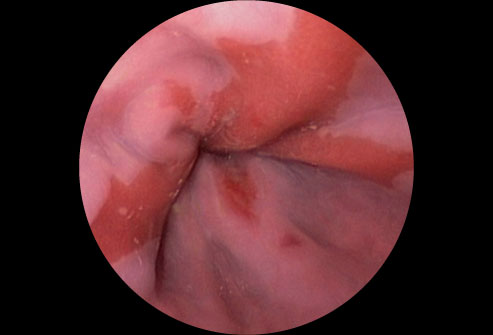
Endoscopy, the use of a minimally invasive fiber-optic camera, to evaluate the inside of the esophagus and/or trachea (windpipe) and lower airways is invaluable for thoroughly evaluating patients suspected to be living with GERD. Although any veterinarian can perform endoscopy with the appropriate equipment, board-certified veterinary internal medicine specialists undergo extensive training to perform these procedures, and partnering with one of them is frequently invaluable to ensure an accurate diagnosis is made.
GERD – How is it treated?
The therapeutic goals for a patient living with GERD are reducing the acidity of stomach fluid and promoting proper gastrointestinal motility. Common interventions to achieve these goals include:
- Dietary Manipulation – Feeding a diet with low fat and moderate protein content helps reduce stomach acid production. Some appropriate diets include Royal Canin Gastrointestinal Low Fat, Hill’s Prescription Diet i/d low fat, Purina OM, Hill’s Prescription Diet w/d. Feeding frequent, small meals may also help control gastric acid production.
- Antacids – Classes of drugs called proton pump inhibitors/PPIs (e.g. omeprazole/PrilosecOTC®) and histamine-2-antagonists (e.g. cimetidine/Tagamet®, famotidine/PepcidAC®, ranitidine/Zantac®) are frequently used to treat patients with GERD. Histamine-2-antagonists do not appear to be as effective as PPIs for raising the pH of stomach fluid, but PPIs given by mouth do not exert their benefits immediately. Serial monitoring is recommended for patients receiving chronic histamine-2-antagonists and/or PPIs.
- Pro-Motility / Esophageal Sphincter Tone Therapy – Drug therapy to improve the tone of the sphincter that connects the esophagus with the stomach (called the lower esophageal sphincter) is often beneficial.
- Protection for Esophageal Mucosa – Administration of a medication called sucralfate is often given as a slurry to coat the lining of the esophagus to provide protection and help prevent progression of the disease.
Employing a multimodal approach to the treatment of a patient with GERD is helpful. Partnering with a board-certified veterinary internal medicine specialist can be instrumental for developing an effective and cost-effective treatment plan. With adequate response to therapy, the goal is to gradually taper and ultimately discontinue medications if clinical signs are appropriately controlled. Medications should be weaned/discontinued one at a time. Complete resolution of clinical signs is not always possible, and some patients require lifelong therapy.
The take-away message about GERD in dogs and cats…
Veterinarians are more frequently recognizing GERD in dogs and cats as a potential cause of discomfort and recurrent chronic clinical signs like coughing, regurgitation, and nasal discharge. After a thorough diagnostic investigation, multimodal therapy is available to help control (and hopefully resolve) clinical signs in the majority of affected patients. Consultation with a board-certified veterinary internal medicine specialist can empower pet parents with the information needed to make informed decisions about diagnosing and treating this condition.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
cgb





