Respiratory distress in dogs and cats is always scary and often frustrating. A common cause is pleural space disease, the accumulation of fluid and/or air between the body wall and the lungs. This week I review this medical condition so pet parents have some familiarity with it. Please consider sharing it with other pet parents so we can spread the word. Happy reading!
Pleural Space Disease – What is it?
The pleural cavity is a potential space between the body wall and the lungs. Under normal circumstances, there is nothing in this cavity. The lungs lay directly against the body wall. Certain diseases cause air and/or fluid to accumulate in the pleural cavity. The name of the condition varies depending on what accumulates in the pleural cavity. Pneumothorax is the term used to describe the accumulation of air within the pleural cavity. Potential reasons for air to accumulate in the pleural cavity include trauma, cancer, and rupture of abnormal lung structures called bullae.
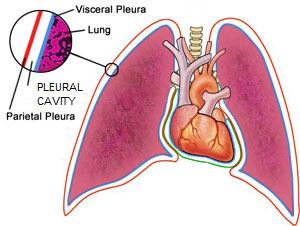
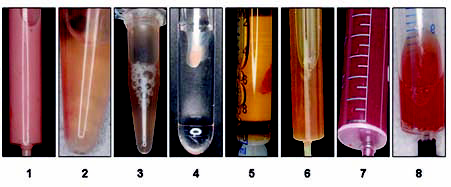
Several diseases can cause fluid to accumulate in the pleural cavity – this is called pleural effusion. Veterinarians categorize the fluid based on protein concentration and cellular components. Categories include
- Transudate – this fluid has a low protein concentration and cell composition
- Modified transudate – this fluid contains a moderate amount of protein and cells
- Exudate – this fluid can be infected (septic) or non-infected (non-septic); a septic exudate is commonly called a pyothorax
- Hemorrhage – this fluid contains protein and cells in similar concentrations as those found in blood; this condition is called a hemothorax
- Chyle – this is fluid that flow through the lymphatic system, and contains a moderate amount of protein with a low-to-moderate cell count; this condition is called a chylothorax
Conditions associated with pleural effusion are:
- Congestive heart failure
- Lung lobe torsion
- Diaphragmatic hernia
- Pancreatitis
- Pulmonary thromboembolism
- Cancers (e.g.: lymphoma, thymoma, mesothelioma, primary lung tumors, metastatic cancers)
- Anticoagulation rat poisons
- Inflammation of blood vessels
- Feline infectious peritonitis (FIP)
- Low albumin level secondary to kidney and/or gastrointestinal diseases
- Lymph vessel obstruction
Pleural Space Disease – What are the clinical signs?
Regardless of whether air or fluid is present in the pleural cavity, patients with pleural space disease typically have the same clinical signs. Most pets develop sudden respiratory distress. The abnormally accumulating fluid and/or air prevents the lungs from properly expanding during inhalation (breathing in). Consequently, affected pets take shallow and rapid breaths. Other signs of pleural space disease include:
- Lethargy
- Reduced (or loss of) appetite
- Exercise intolerance
A veterinarian will thoroughly evaluate patients with suspected pleural space disease. Common physical examination findings include the previously mentioned shallow rapid breathing, as well as anxiety/distress, panting, blue/grey gums and tongue, and muffled heart and lung sounds.
Pleural Space Disease – How is it diagnosed?
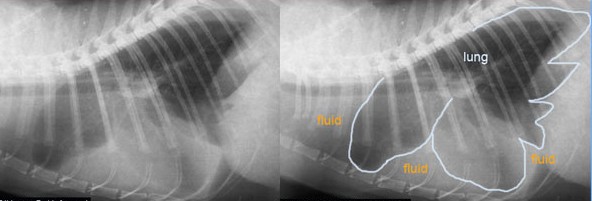
A patient’s cumulative history and physical examination findings frequently provide veterinarians with enough information to have a very high index of suspicion that a patient is living with pleural space disease. Radiographs (x-rays) readily show air and/or fluid in the pleural cavity. Ultimately a minimally invasive procedure called a thoracocentesis (also called a pleurocentesis or a chest tap) must be performed to remove fluid and/or air from the pleural cavity.
Your family veterinarian may recommend evaluation by a board-certified veterinary internal medicine specialist or board-certified veterinary emergency and critical care specialist to help determine the cause of your pet’s pleural space disease and to develop an appropriate treatment plan. However, patients in respiratory distress should be stabilized prior to transport to a referral/specialty hospital. While family veterinarians may be logically inclined to refer your pet immediately, transporting an unstable patient in respiratory distress can be lethal. Thus your family veterinarian will perform a thoracocentesis to stabilize an unstable pet before transport to a referral/specialty hospital.

Pleural Space Disease – How is it treated?
The initial treatment for a patient with pleural space disease is removing air and/or fluid from the pleural cavity. As mentioned earlier, the pleural cavity is evacuated via a minimally invasive procedure called a thoracocentesis; thus this procedure is both diagnostic and therapeutic. After performing a thoracocentesis, chest radiographs (x-rays) are reevaluated to look for an underlying cause since the lungs are now better able to expand. Some patients require more than one thoracocentesis, and those who require multiple chest taps often benefit from the placement of a thoracostomy tube (also called a chest tube).

Any fluid should be evaluated for protein content and cell composition. Initially evaluating pleural effusion under the microscope in the hospital is helpful, but a sample should also be sent to a reference veterinary laboratory for evaluation by a board-certified veterinary clinical pathologist. Patients are provided supplemental oxygen to help them breathe with improved comfort. Additional therapies should be tailored to the underlying cause of the fluid and/or air accumulation in the pleural cavity. Some diseases are more treatable than others, and the key to maximizing a positive outcome is evaluation by a veterinarian as soon as possible.
The take-away message about pleural space disease…
In normal dogs and cats, there is nothing between the lungs and the body wall. However, a variety of diseases cause fluid and/or air to build up in this location called the pleural space. Patients with pleural space disease often experience marked respiratory distress and are at risk for sudden death. Timely and efficient diagnostic investigation and therapeutic intervention are absolutely essential for maximizing the likelihood of a positive outcome.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
cgb




