Last week I reviewed some common emergency situations for which you should bring your cat to the emergency room. Of course, we can’t forget about our canine companions! So, this week I focus on specific scenarios that necessitate emergency care for your pooch. Happy reading!
Pooch Plight #1 – Non-Productive Vomiting
Dogs vomit for myriad of reasons – infections, gastrointestinal foreign bodies, liver disease, kidney disease, etc. Certainly, it’s imperative to work with your family veterinarian to determine the cause of a pet’s vomiting to ensure proper treatment is initiated. There is one specific scenario I want all dog parents to recognize as an immediate and life-threatening emergency. What is it? Families should seek veterinary care as soon as possible if their dog vomits but doesn’t bring anything up. We call this non-productive retching. Think dry heaves.
Non-productive vomiting or retching is a major red flag for a life-threatening emergency called gastric dilatation-volvulus (GDV). The more commonly used term for GDV is bloat, and this problem is a surgical emergency. Without prompt stabilizing care and subsequent surgery, affected dogs will die. But there’s good news. With prompt intervention, dogs can make a meaningful recovery and lead high quality of lives with their families. To learn more about GDV, click here.
Pooch Plight #2 – Vulva Discharge
The vast majority of owned dogs in the United States are spayed (not spaded – that would hurt!), meaning they have surgically had their ovaries and uterus removed so they can’t reproduce (a surgery called an ovariohysterectomy or OVH). While we are still learning about the best time to spay female dogs, there is no doubt OVH is recommended for all dogs not intended for responsible breeding.

A situation about which I want parents to recognize as a potential emergency is the presence of discharge appearing at the vulva of an intact female dog. Why is such a discharge concerning? It’s a red flag for a uterine infection called pyometra. Essentially, the uterus becomes filled with a large volume of purulent exudate, otherwise known as pus. A pyometra is considered a surgical emergency. Indeed, in veterinary school I was taught to “never let the sun set on a pyometra.” Occasionally, pyometra patients intended for breeding can be treated with aggressive medical therapy, but surgery (spaying) is absolutely the preferred curative intervention. With prompt stabilization and surgery, dogs can make a complete recovery and return to high quality lives. To learn more about pyometra, click here.
Pooch Plight #3 – Seizures
Just as for cats, dogs can experience seizures too. As you may recall from last week, seizures may be caused by one of the following:
- Metabolic disease / organ dysfunction
- Central nervous system disease
- Epilepsy
Dog parents should work diligently to accurately determine the cause of their dog’s seizures so the most appropriate therapies can be initiated. There are some distinct situations involving seizures for which pets should be evaluated by a veterinarian as soon as possible:
- More than two (2) seizures in a 24-hour period – this is called a cluster event
- Any seizure that lasts more than five (5) minutes and then stops
- Any seizure that doesn’t stop – this is called status epilepticus
To learn more about seizures, click here.
Pooch Plight #4 – Trauma
Although curiosity has been known the kill cats, dogs can be mischievous too. Their mischief can get them into trouble, sometimes life-threatening situations. Motor vehicle accidents, hunting mishaps and other gun & bow/arrow mishaps, animal fights, broken bones, etc. These scenarios are unfortunately fairly common, and the vast majority of pet parents know to seek immediate veterinary care. Here’s the point about traumatized dogs – get them to your closest veterinary hospital as quickly and as safely as possible.
Pooch Plight #5 – Collapse
Earlier I discussed specific reasons to bring dogs with seizure activity to the emergency room. When dogs have generalized seizures, they typically collapse because of their uncoordinated muscle activity. There are other reasons for animals to collapse that are similarly emergencies, and I believe it’s important for dog parents to know about them too.
A major reason dogs collapse is due to underlying heart disease. Such a collapse is called syncope (pronounce sink-o-pee), and it’s caused by a sudden decrease in oxygen delivery to tissues (including the brain) because of an acute drop in blood pressure. Syncopal episodes are often very challenging to distinguish from seizures even for board-certified veterinary neurologists and cardiologists. If possible, video recording a collapse episode can provide invaluable information to your pet’s veterinary healthcare team. It’s imperative pet parents safely and quickly transport their dog to a veterinary hospital for evaluation and medical intervention.
Another common reason dogs collapse is because of internal bleeding. A classic scenario is a pet parent taking their dog on a walk through the neighborhood. As they work their way back home, the dog stops, lays down, and then refuses to walk anymore. Sure, the fur baby may just be tired. But this scenario immediately raises concerns for internal hemorrhage. It can be challenging for a pet parent to know if their dog’s refusal to walk any more is due to internal bleeding, but there are some things they can check to get more information, including:
- Check heart rate – count the number of heart beats in 15 seconds and multiply this number by 4. If the product is persistently greater than 130 for large & giant breeds / 150 for medium and small breeds, the pet should be evaluated by a veterinarian as soon as possible
- Check the color of the gums – if the gums are pale pink or white, this may indicate blood loss has occurred. Such patients should be evaluated by a veterinarian as quickly as possible
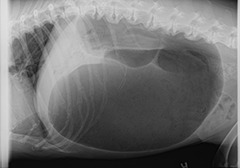
Pooch Plight #6 – Trouble Breathing
Oxygen is essential for life. When dogs have difficulty breathing (called dyspnea; pronounced disp-nee-ah), they can’t get enough oxygen into their lungs or from their lungs into the bloodstream to be delivered to vital organs. There is a plethora of reasons for which dogs can’t breathe normally, including laryngeal paralysis, brachycephalic airway syndrome, congestive heart failure, chronic bronchitis, and various types of pneumonia. Patients who can’t breathe normally should be evaluated by a veterinarian as soon as possible, even if in the middle of the night. Time is of the essence, and without medical care, dogs with respiratory difficulties can die.
Below are some things pet parents can evaluate to help them decide if they should seek veterinary care:
- Resting respiratory rate – measure the number of breaths a dog takes in 15 seconds. Multiply the number by 4. If the product is more than 50, you should take your dog to the closest veterinarian as quickly and as safely as possible.
- Cyanosis – if your dog’s gums, lips, and/or tongue are blue/grey/purple, seek immediate veterinary care at the closest veterinary hospital
- Sitting in unusual positions – Sometimes when you’re having trouble breathing, it’s more comfortable to sit in a specific position. For example, when you’re congested, sitting with your head propped up on a lot of pillows often provides some relief. Sometimes, sitting in a specific posture is more comfortable for dogs having difficulty breathing. This phenomenon is called orthopnea.
Pooch Plight #7 – Toxin Ingestion
Dogs are perpetually surrounded by potential toxins. Compounding this exposure is the fact dogs like to put anything and everything in their mouths. One of my favorite poems can be found in the book, Unleashed: Poems by Writers’ Dogs, by Amy Hempel and Jim Shepard. In the book, a Labrador Retriever named Birch shares a poem translated by his mom:
You gonna eat that?
You gonna eat that?
You gonna eat that?
I’ll eat that.
This poem highlights the fact dogs will eat anything. Some of the most common intoxications in canine medicine are ethylene glycol (antifreeze), household cleaners, xylitol, chocolate, poisonous plants like Sago Palms, poisonous foods/fruits like grapes/raisins & alliums, rodenticides (anticoagulant & bromethalin), and non-steroid anti-inflammatory drugs (NSAIDs). If you suspect or know your dog has been exposed to a toxin chemical or substance, please seek immediate veterinary medical attention for them. Pet parents may find it helpful to contact the ASPCA Animal Poison Control Center. For a nominal fee, you can speak with a veterinary toxicology expert for initial advice. If your pet does require veterinary care, your pet’s doctor can subsequently speak with the toxicologist to help ensure your pet receives the best possible care. When you bring your pet to the veterinary hospital for care, please remember to bring the package that contained the toxin – the information contained on the packaging can be very helpful to your pet’s healthcare team!
The take-away message about when to bring your dog to the ER…
Emergencies happen. They are an inevitability for pooches and their families. So, it’s imperative pet parents are prepared for them, that they know what constitutes an emergency, and they know when to see immediate veterinary medical care.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
Wishing you wet-nosed kisses,
CriticalCareDVM