Last week I reviewed a relatively unknown household threat to dogs and cats – bread dough intoxication. More commonly around the holidays emergency rooms see a spike in a specific type of illness in our furry companions – acute pancreatitis. This illness can manifest at any time of year, but incidence around the major winter holidays in the United States is so high that many refer to the days after Thanksgiving and Christmas as “pancreatitis days.” Given the time of year, this week I’m dedicating some blog space to highlight this disease so pet parents can be as informed as possible. Happy reading!
Acute Pancreatitis – What is it?
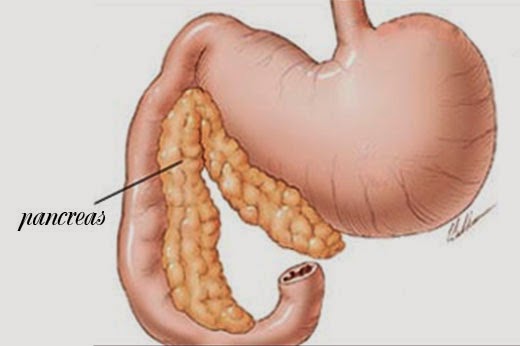
The pancreas is a boomerang-shaped organ in the abdominal cavity that has a number of important functions. One of these vital jobs is to make and secrete specific enzymes that help the body digest food, particularly fats and carbohydrates. Occasionally the pancreas becomes inflamed, and this is called pancreatitis. The body tries to isolate the inflammation to just the region around the pancreas, but often times the body’s defense mechanisms are overwhelmed, allowing inflammatory chemicals to spread to other parts of the body to cause dysfunction at those sites.
Several risk factors for acute pancreatitis in dogs and cats have been identified (see Table #1):
| Table 1: Risk Factors for Development of Acute Pancreatitis in Dogs and Cats | |
| Breed / Pedigree | Dogs: Miniature Schnauzers, Dachshunds, Poodles, Cocker Spaniels, Fox Terriers, Laikas, Alaska Malamutes
Cats: Siamese, Domestic Shorthair |
| Biochemical | Dogs: high triglyceride and cholesterol levels, high blood calcium
Cats: high blood calcium |
| Reproductive status | Dogs: spayed/castrated |
| Body Condition | Dogs: overweight, obese |
| Concurrent Metabolic Disorders | Dogs: diabetes mellitus, chronic kidney disease, neoplasia, congestive heart failure, autoimmune disorders, inflammatory bower disease
Cats: inflammatory bowel disease, inflammatory liver disease (e.g.: cholangiohepatitis) |
| Age | Dogs: >7 years |
| Nutrition | Dogs: ingestion of unusual food items, getting into trash, ingestion of table scraps |
| Infections | Cats: Liver flukes (e.g. Eurytrema procyonis, Amphimerus pseudofelineusI) toxoplasmosis, calicivirus |
| Miscellaneous | Dogs: previous surgery other than neutering
Cats: bile reflux, duodenal reflux
Both: common bile duct obstruction, ischemia, pancreatic tumors |
| Medications | Dogs: azathioprine, potassium bromide, sulfonamides, N-methyl- glucamine, anticholinesterases, L- asparaginase
Cats: Organophosphates |

Acute Pancreatitis – What are the signs of it?
A classic scenario during the winter holidays is a dog that gets into the trash, ingesting some fatty morsel of scrumptiousness. In a variable period of time (e.g.: a few hours to a few days), the pet develops signs of gastrointestinal distress. One should know dogs and cats with acute pancreatitis do not have the same clinical signs. In other words, cats are not small dogs, and one needs to be aware of the differences between these species.
Many affected dogs have a mild, self-limiting course of disease. Some never even show signs of being sick. Indeed, many dogs go undiagnosed! Middle-aged females are more likely to develop acute pancreatitis than other patient populations. The most common clinical signs in dogs are:
- Dehydration (97%)
- Loss of appetite (91%)
- Vomiting (90%)
- Weakness (79%)
- Abdominal pain (58%)
- Obesity (43%)
- Diarrhea (33%)
- Fever (32%)
- Jaundice/icterus (32%)
In contrast to dogs, the most common clinical signs in cats are a reduced (or complete loss of) appetite (63-100%) and lethargy (50-100%). Cats infrequently vomit (35-52%) and rarely develop a fever (7%). Other reported clinical signs include:
- Dehydration (33-92%)
- Increased thirst & frequency of urination (20%)
- Diarrhea (11-15%)
- Weight loss (33%)
- Elevated respiratory rate (74%)
- Low body temperature (68%)
- Elevated heart rate (48%)
- Abdominal discomfort (9-25%)
- Jaundice/icterus (16-64%)
- Difficulty breathing (20%)

Approximately one quarter of cats will have a palpable abdominal mass, and this may be misdiagnosed as enlarged lymph nodes in the abdominal cavity or being associated with the intestinal tract.
Potential life-threatening complications in both dogs and cats include an inability to clot blood properly, abnormal heart rhythms, blood infection, acute kidney injury (AKI), pleural effusion (fluid accumulation between the body wall and lungs), and “water on the lungs” (called pulmonary edema). Acute pancreatitis may also be associated with transient or permanent diabetes mellitus in cats and less commonly in dogs.
Acute Pancreatitis – How is it diagnosed?
The gold-standard method for diagnosing acute pancreatitis in dogs and cats is obtaining a biopsy of the pancreas. However, this is an invasive surgery, and many patients with this disease are not stable enough to undergo general anesthesia for a biopsy procedure. Thus after obtaining a complete history and performing a thorough physical examination, a veterinarian will perform a logical series of initial tests that typically includes:
- Complete blood count: a non-invasive blood test that gives information about red blood cells, white blood cells, and cells that help blood clot properly (called platelets)
- Serum biochemical profile: a non-invasive blood test that gives information about electrolytes (e.g.: sodium, potassium), liver function, some gastrointestinal enzymes, and kidney function
- Urinalysis: a non-invasive evaluation of urine to help evaluate kidney function, as well as to screen for inflammation, excess protein, and infection
- Pancreas-specific tests: there a several non-invasive blood tests that can help identify pancreatic inflammation. Possible options include the SPEC fPL™, SPEC cPL™, SNAP cPL™, SNAP fPL™, and PrecisionPSL™
Additional blood and urine testing may be recommended based on a patient’s history and physical examination. Diagnostic imaging is a very useful tool for helping to diagnose and monitor patients with pancreatitis. A variety of imaging modalities may be utilized for patients living with acute pancreatitis. The two most common are abdominal radiography (x-rays) and ultrasonography:
- Abdominal Radiography (x-rays): Abdominal radiography is widely available, safe, and non-invasive. This modality is justified to rule out some causes of vague gastrointestinal signs. However radiographic changes consistent with pancreatitis are often quite subtle. As such, a veterinarian can not make a conclusive diagnosis of acute pancreatitis based on abdominal radiography alone.
- Abdominal Ultrasonography: When performed by an extensively-trained and experienced ultrasonographer (e.g.: board-certified veterinary radiologist or board-certified veterinary internal medicine specialist), ultrasonography is non-invasive technique that is superior to radiography for identifying acute pancreatitis.
Partnering with a board-certified veterinary internal medicine specialist or board-certified veterinary emergency and critical care specialist early in the course of a pet’s disease can be instrumental in developing an efficient and cost-effective diagnostic plan for an affected fur baby.
Acute Pancreatitis – How is it treated?
In my mind, I put pancreatitis on a scale from one to ten. Ones are patients who need minimal supportive care at home. Tens are those fighting for their lives in the intensive care unit (ICU).
To date there is no specific treatment for acute pancreatitis.
There is no antidote for this disease. All therapeutic interventions are aimed at preventing escalation of the scale – to prevent a two from becoming an eight. Overall, treatment of acute pancreatitis has two main goals:
- Correcting any underlying predisposing factor(s)
- Reducing pancreatic inflammation
Adequate pain management is of paramount importance. Many patients require more than one pain medication, and often benefit from around-the-clock intravenous infusions in a referral hospital setting. The routine use of antibiotics is a controversial topic when treating patients with acute pancreatitis; a veterinarian will thoroughly evaluate a pet’s history and laboratory results to help determine if antibiotic therapy is warranted. The extensive inflammation in and around the pancreas commonly induces nausea and vomiting, and slows down (and sometimes stops) the normal movement of the gastrointestinal tract (called peristalsis). Thus affected patients frequently benefit from anti-nausea/anti-vomiting drugs, as well as those medications that promote normal gastrointestinal movement.
Nutritional support is absolutely essential for maximizing a successful outcome.
Feeding patients with acute pancreatitis should be implemented as soon as possible.
Historically, prolonged fasting (more than 3 days) was advocated to avoid stimulation of the pancreas. However we now know this approach is not in a patient’s best interest. Few reasons exist to justify withholding nutrition from a pancreatitis patient, and once these issues have been addressed, nutritional support should be instituted immediately. Placement of a temporary feeding tube to provide early nutrition should be considered as an almost mandatory aspect of effective treatment. Force/coax feeding is not recommended because it readily promotes food aversion, a scenario where a pet who feels well enough to eat after recovering but will not eat because of the negative experience of force/coax feeding.

The majority of canine patients with mild-to-moderate acute pancreatitis respond favorably to a veterinarian’s interventions. However those living with severe manifestations of this disease often experience complications, and can succumb to the disease. Prognosis is typically variable for cats with acute pancreatitis. Some laboratory changes have been associated with a poor prognosis in cats, including low blood calcium, high blood potassium, respiratory distress, and a severely elevated SPEC fPL™. Early partnering with a board-certified veterinary internal medicine specialist or board-certified veterinary emergency and critical care specialist can help maximize the likelihood of successful outcome.
The take-away message about acute pancreatitis…
Severe inflammation of the pancreas called acute pancreatitis is a disease that can be life-threatening if not identified and treated efficiently and effectively. This malady often manifests after pets ingest fatty meals or foods to which they are not accustomed. Many risk factors also exist for both dogs and cats that increase the risk for developing acute pancreatitis. Blood, urine, and diagnostic imaging tests help veterinarians accurately diagnose this disease. Once identified and depending on the severity of clinical signs, patients may require supportive care at home or aggressive critical care in an ICU setting. Consultation with a board-certified veterinary internal medicine specialist or board-certified veterinary emergency and critical care specialists can help a fur baby successfully win the battle against acute pancreatitis.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
To find a board-certified veterinary emergency and critical care specialist, please visit the American College of Veterinary Emergency and Critical Care.
Wishing you wet-nosed kisses,
cgb




