Proper nutrition is uniquely important for cats. They are obligate carnivores, meaning they require animal-based protein as part of their diet. When cats become ill, they often lose their appetites. Yet by foregoing their meals, our feline friends put themselves at risk for a potential lethal liver problem called hepatic lipidosis. This week I share some informative morsels about this condition. Happy reading!
Hepatic Lipidosis – What is it?
Hepatic lipidosis is one of the most common liver diseases in cats in the United States. Healthy cats have lipid (fat) in 5% of their liver tissue. The livers of cats with hepatic lipidosis have lipid in more than 50% of their livers. This fat is stored in unique structures called vacuoles. When vacuolization reaches a critical point, normal cellular metabolism is disrupted to results in liver dysfunction.
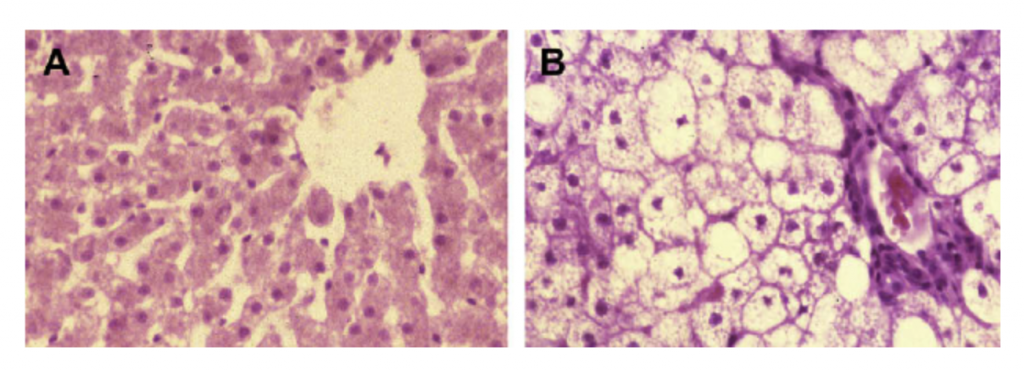
A. Liver biopsy from a healthy 2-year old cat. B. Liver biopsy from a 2- year old cat with hepatic lipidosis. Note the diffuse vacuolization. Image courtesy of Dr. PJ Armstrong.
Hepatic lipidosis can occur on its own (primary) or in combination with other conditions (secondary). Factors that have been associated with the development of this syndrome are:
- Overweight & obesity
- Anorexia
- Diet changes
- Environmental stress
- Cancer
- Diabetes mellitus
- Hyperthyroidism
Both ideal weight and overweight/obese cats may develop hepatic lipidosis when nutritionally intake is reduced. It is important to note the necessary period of reduced food intake and the degree of weight loss for primary hepatic lipidosis appears to be ~5-7 weeks and 30-35%, respectively. However, secondary hepatic lipidosis appears to develop more rapidly.
Veterinarians do not yet fully understand the mechanism(s) for the development of hepatic lipidosis. Some popular theories include deficiencies in carnitine, glutathione, cobalamin/vitamin B12, and hormones & fatty acids responsible for fat metabolism (i.e. orotic acid, hormone-sensitive lipase, lipoprotein lipase). Regardless of cause, liver failure occurs when lipid vacuolization results in more than 70% liver dysfunction.
Hepatic Lipidosis – How is it diagnosed?
Cats with hepatic lipidosis typically have a history of anorexia, weight loss, and lethargy. Intermittent vomiting is also common. Veterinarians initially frequently document dehydration, an enlarged liver, and icterus (yellowing of the skin and sclera/whites of the eyes). Severely affected pets can have fluid accumulation in their abdominal cavities, as well as bleeding disorders and a neurologic syndrome called hepatic encephalopathy.

Board-certified veterinary internal medicine specialist Dr. Kristopher Sharpe performs an abdominal ultrasound exam on a cat.
(Press Photo/Lance Wynn)
Veterinarians will initially perform non-invasive blood and urine tests to help determine an underlying cause of pet’s illness, as well as expected complications of hepatic lipidosis (i.e.: hypokalemia/low potassium, hypoglycemia/low blood sugar). Ultimately to diagnose hepatic lipidosis, the doctor will perform an abdominal ultrasound and sample liver tissue. Click here to review a previous post discussing liver sampling.
Hepatic Lipidosis – How is it treated?
The mainstay of treatment is providing adequate nutrition. Unfortunately, cats with this disease either won’t eat enough calories or at all. Mildly affected pets may respond adequately to an appetite stimulant and/or anti-nausea medication(s). Most require more intervention to realize a successful outcome. Specifically, the placement of a temporary supplemental feeding tube can truly be lifesaving for cats with hepatic lipidosis since recovery generally takes 12-16 weeks.
Use of an esophagostomy tube – a temporary feeding tube placed into the esophagus during a brief period of anesthesia – is the most common way to provide nutrition to affected cats during the treatment period. Pet parents use this type of food to provide meals and medications until a cat begins consistently eating well on its own. Force feeding cats is not recommended. Such an intervention readily promotes food aversion.
Imagine being nauseated for any number of reasons. Now imagine having someone shove food down your throat. Understandably this would be a very negative experience, and you likely would never want to eat that forced food again. The same thing happens to force fed cats. One of my stellar professors in veterinary school always told us, “If you can do better, do better!” In terms of feeding cats with hepatic lipidosis, we can absolutely do better than force feeding by using temporary supplemental feeding tubes!
In addition to an adequate amount of calories, cats with hepatic lipidosis also benefit from various supplements, including:
- Cobalamin / vitamin B12
- s-adenosylmethionine (SAM-e) – a potent anti-oxidant and glutathione donor
- Taurine
- Potassium
- L-carnitine – helps with fatty acid transport and reduces fat accumulation in the liver
- Various other vitamins (C, E, K1)
Collaborating with a board-certified veterinary internal medicine specialist can be invaluable for formulating the most appropriate treatment plan for a cat living with hepatic lipidosis.
The take-away message about hepatic lipidosis in cats…
Hepatic lipidosis, often called fatty liver syndrome, is a common liver disease in cats who don’t eat an adequate quantity of appropriate calories. This disease may occur by itself or in conjunction with other serious disorders. Definitive diagnosis requires sampling of the liver. Treatment is via provision of adequate nutrition and supplementation of various vitamins and liver supportive nutraceuticals.
To find a board-certified veterinary internal medicine specialist, please visit the American College of Veterinary Internal Medicine.
Wishing you wet-nosed kisses,
cgb


