This morning as I was driving home from my own acupuncture appointment for an orthopedic issue, I realized it’s been some time since I posted information about orthopedic conditions in dogs and cats. The musculoskeletal system is so important, so this week I’m sharing some tidbits about an inflammatory cartilage condition called osteochondritis dissecans (also known as osteochondrosis dissecans and OCD). I hope you find the material helpful and share-worthy. Happy reading!
Osteochondritis Dissecans – What is it?
Cartilage is a strong yet flexible supporting tissue found throughout the body. It provides the framework of some organs like the nose, larynx (voice box) and trachea (windpipe). Cartilage also forms the articulating surfaces of bones like the humerus (upper arm bone). An articulating surface is any surface of a skeletal structure that makes direct contact with another skeletal structure. Cartilage doesn’t have its own blood supply, and rather receives nutrients through diffusion from nearby capillaries.
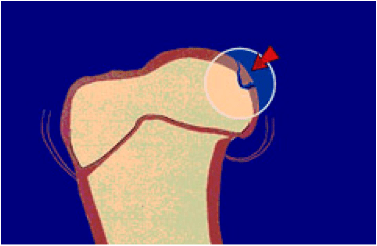
Common location of an OCD lesion in the head of the humerus. Illustration courtesy of the American College of Veterinary Surgeons.
Bone tissue is created through two processes during fetal development – intramembranous ossification and endochondral ossification. The latter is essential for the formation of long bones, the growth of these bones, and natural healing of fractures. When endochondral ossification is disturbed, cartilage at the end of long bones is damaged and fails to mature into bone. The result is a focal area of cartilage thickening that is susceptible to injury. Frequently, a fissure develops in the abnormal cartilage, allowing synovial fluid (joint fluid) to get under it. As more synovial fluid seeps under the abnormal cartilage, a piece of abnormal cartilage can partly break away to create a flap. Most severely, the dissecting flap of cartilage can dislodge into the joint – this is called a joint mouse.
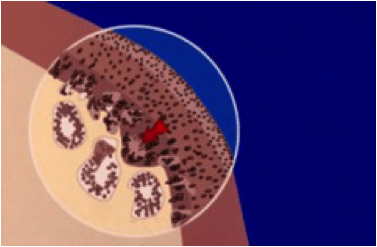
Abnormal endochondral ossification results in inappropriate thickening of articular cartilage. Illustration courtesy of the American College of Veterinary Surgeons.
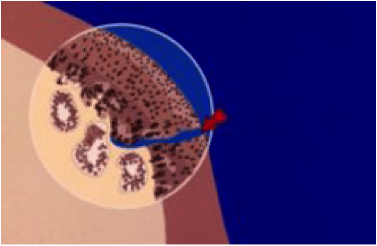
Cartilage thickening creates fissures in the cartilage, ultimately leading to the formation of a flap. Illustration courtesy of the American College of Veterinary Surgeons.
To date, veterinarians don’t know the exact cause of OCD. Several factors have been implicated, including:
- Rapid growth
- Trauma
- Hormones
- Genetics
- Over-nutrition
- Excessive dietary calcium & protein
Osteochondritis Dissecans – What does it look like?
Young (3- 9 months of age) large and giant breed dogs are over-represented for developing OCD:
- Saint Bernards
- Rottweilers
- Newfoundlands
- Mastiffs
- Old English sheepdogs
- Standard Poodles
- Chow Chows
- Labrador retrievers
- Great Danes
- Golden retrievers
- Bernese Mountain dogs
- Bull terriers
- German Shepherd dogs
However, some breeds – Doberman pinschers, Collies, and Siberian huskies – rarely develop this disease. Affected dogs are typically lame and are reluctant to exercise. Males are more affected than females. Clinical signs may be mild or severe, as well as intermittent or constant. The most commonly affected joints are the shoulders, elbows, and tibiotarsal joints (also known as the hocks or ankles).
Osteochondritis Dissecans – How is it diagnosed?
After performing a thorough physical examination, a veterinarian will need to perform to diagnostic imaging. Most commonly, they will evaluate radiographs (x-rays). Often patients need to be sedated to obtain the appropriate views because extending and flexing affected joints can be painful.
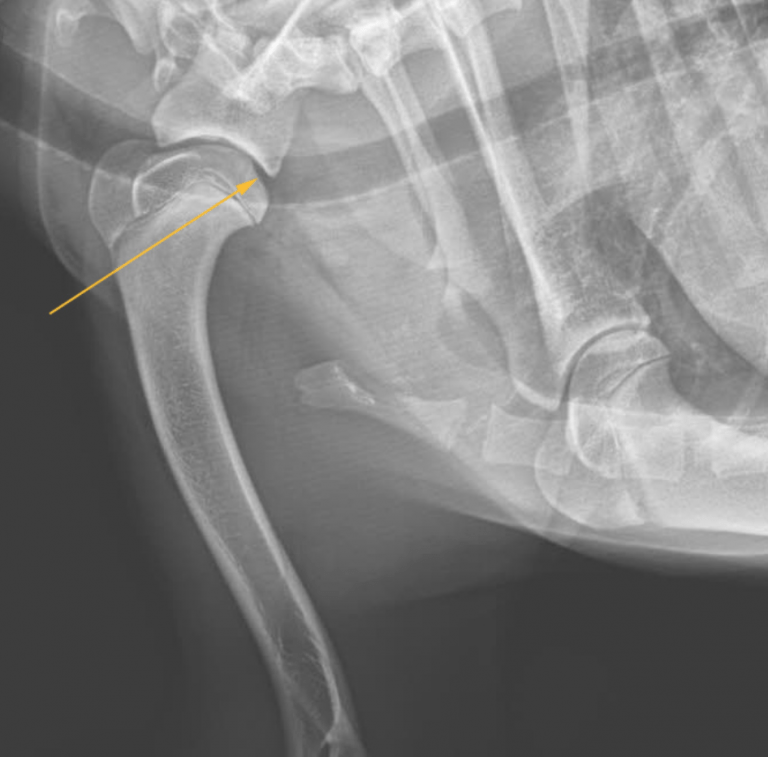
The yellow arrow points to an OCD lesion in the shoulder joint of a dog. Image courtesy of Dr. Alexandria Durfy
Occasionally, radiographs are not diagnostic, and other forms of imaging are needed. These modalities may include:
- Arthrography – the injection of a contrast agent into a joint to highlight cartilage defects
- Magnetic resonance imaging (MRI)
- Arthroscopy – the use of a fiber-optic camera to directly look inside an affected joint
Osteochondritis Dissecans – How is it treated?
Treatment is variable depending on whether a dissecting flap of cartilage has formed in a joint. If no flap has formed, some patients may improve with temporary (2-4 weeks) exercise restriction, non-steroidal anti-inflammatory (NSAID) therapy, and multimodal pain management. Most patients benefit from surgery, and clinical studies suggest early surgical intervention in young patients has the best outcomes.
The goals of surgery are to remove all loose fragments of cartilage within the joint are removed. The defect in the cartilage is curetted (scraped) until the underlying bone begins to bleed. This process stimulates the defect to heal through the formation of fibrocartilage. These surgical goals can be achieved either through an arthrotomy (surgical opening of a joint) or the use of arthroscopy. The latter is an alternative minimally invasive procedure associated with shorter recovery times; furthermore, bilateral arthroscopic procedures are also possible. Please view the video below to see arthroscopy of a dog’s shoulder joint that has an OCD lesion.
A relatively new intervention for the treatment of OCD is a procedure called an osteochondral autograft transfer. Pieces of cartilage and cancellous bone are harvested from non-weight bearing areas of the affected joint and are subsequently transplanted into the OCD defect. This procedure is essentially a restructuring of the articular surface. Pet parents will likely find it helpful to consult with a board-certified veterinary surgeon to determine the best course of treatment for their dog.
Following surgery (arthrotomy or arthroscopy), 75% of dogs with shoulder OCD will have no signs of lameness. Approximately 20-22% will have persistent lameness, and ~2% have persistent lameness. Most dogs with stifle and tibiotarsal OCD are more comfortable after surgery, but complete resolution of lameness is unlikely.
The take-away message about osteochondritis dissecans in dogs…
Osteochondritis dissecans is an orthopedic condition characterized by abnormal articular cartilage formation in a joint. Affected pets are typically lame, painful, and reluctant to exercise. Early identification and surgical intervention is recommended.
To find a board-certified veterinary surgeon, please visit the American College of Veterinary Surgeons.
Wishing you wet-nosed kisses,
CriticalCareDVM


DVM2
Excellent Article! Thanks 🙂
CriticalCareDVM
Thank you so much! I’m glad you found it helpful.
Anna
Great article Chris.
CriticalCareDVM
Thanks so much!